Seed oils are NOT causing colorectal cancer.
Media clickbait and wellness influencers are lying about a recent study that didn't even look at potential dietary impact in colorectal cancer.
The fear-baiting is truly out of control these days. I can’t open a web browser or social media app without seeing a wildly mischaracterized headline or meme from a wellness influencer that is intended to cause fear about science or health topics.
Most recently? Blatantly false headlines and social posts claiming seed oils are causing colon cancer.
No - a new study did NOT say that colorectal cancer is caused by seed oils.
In fact, the study didn’t look at any sort of dietary contributors in the context of colorectal cancer, seed oil, ultraprocessed foods, or otherwise.
I’ll repeat it: there was NO assessment that related to dietary composition and the analysis of tumor samples in this study.
But of course, medical conspiracists and sloppy journalists who clearly didn’t even read the paper - or perhaps even the interview with the lead author - are lying to people. Why? To create fear. We live in a fear economy so if they can scare people, they can sell them something.
Whether or not people are terrified of seed oils has zero impact on me personally. But these grifters have no understanding of basic metabolic processes, cancer biology, and cellular signaling pathways, and as such, their lack of science literacy is impacting their followers.
And I believe that people who have no expertise in a topic have no business speaking on the topic - and certainly no business manipulating fundamental concepts to profit off of others. So let’s get into it.
What is this “new study” even about?
The study in question being propagated by your local anti-seed oil influencers was published in Gut, of the British Medical Journal.
In a nutshell: the study took frozen 40 frozen colorectal cancer biopsies and matched non-cancer biopsies (tissue in the same patient ~10 cm from the tumor), and processed them to conduct a variety of molecular analyses.
Molecular analyses means researchers are trying to parse out things going on at the molecular level to create hypotheses about pathology of colorectal cancer.
In this study, these molecular analyses include:
Analytical chemistry analysis of lipids involved in metabolic and signaling pathways of cells. They use a method called LC-MS/MS (Liquid chromatography–tandem mass spectrometry), a technology that separates chemicals in a sample and analyzes them based on electrical charge to create a molecular fingerprint in order to identify each chemical in a sample.
Gene expression using two techniques: microarray - which looks at a pool of expressed genes (mRNA transcripts) extracted from cells, and spatial transcriptomics - a method where the physical structure of the tissue is preserved to look at regions where genes might be expressed in higher or lower quantities.
I chuckled because Affymetrix was the first microarray I used over 15 years ago.
This paper is a hypothesis-generating study.
The researchers used clinical samples for brute-force techniques to gather large data sets to assess patterns that differ between cancer biopsies and normal tissue biopsies. They form ideas about WHAT may be involved mechanistically based on those observations, to conduct future studies to assess the credibility of those ideas.
It’s important to understand that:
The data cannot tell them any mechanisms of cancer, because they are a single snapshot in time.
The data cannot tell them of causes of cancer, because this is observational.
The data cannot tell them of functions of these molecules in the context of cancer, because there is no control of the environment.
Everything in this study is observational. It was not a clinical trial looking at changes in cancer as a result of dietary composition or intervention.
More than that, there was no information about patient diet, no long-term or longitudinal data to assess impact of dietary factors on patterns they observed, or even if diet is involved.
I’ll repeat it: nothing in this study factored in what a patient ate in the context of the biopsy samples or the cancer itself.
Patient samples were from mostly people over 50.
The mean age was 64 (range 30-85). While we don’t have the full age distribution, the mean age of 64.025 ± standard deviation of 13.08, and a range of 30-85 tells us that 68% of the values are between 50.95 and 77.12 - which means 68% of the patients were between the ages of 51 and 77. Which makes sense because 80% of all cancers occur in adults 50 and older.
This study had nothing to do with seed oils or even dietary contributions to CRC whatsoever, AND it wasn’t specific to “young people” either.
I’m not taking issue with the study itself - it’s a fine exploratory study, with acknowledged and obvious limitations. But that’s exactly what it is: an exploratory study to generate ideas.
So why are wellness influencers trying to link this paper to seed oils (and young people) when the study isn’t about any of that?
The people in question are folks like chiropractor Will Cole, conspiracy theorist Vani Hari, predatory practitioner Leah Connealy, and the wellness ecosystem who make money demonizing seed oils.
And since these individuals don’t understand basic cell biology, they see the word lipids in a media story and immediately jump to the false assumption that these lipids must be directly linked to fats a person physically ate. And then they see in media articles that some of the lipids identified in this large-scale lipid analysis are involved in the arachidonic acid pathway, so they make several more jumps to get to seed oils.
Wellness influencers and media outlets demonize seed oils because they don’t understand basic immunology and cell biology.
I’m going to walk you through their logic - remember: they are on a fishing expedition to vilify seed oils.
Their target is arachidonic acid (AA), because AA and the AA pathway are involved in creating lipid signaling molecules involved in various inflammatory processes, including immune responses. Products of the AA pathway include prostaglandins (like PGE2), critical chemical mediators of pain, fever, and inflammation as well as leukotrienes (like LTB4) which aid in immune cell recruitment and activation of inflammatory pathways.

But of course, remember, these folks don’t know cell biology or immunology. They don’t realize these chemicals are essential for many different physiological processes, including wound healing, response to infection, and general cell function. But they see the word “inflammation” and they think: bad. Even though inflammatory processes are always occurring in our bodies, are regulated, and are essential.
But they claim arachidonic acid is inflammatory - and thus, evil. That’s false.
Arachidonic acid is essential for life. It’s a key component of every one of our cells - specifically, the cell membrane. Each of our cells has a phospholipid bilayer membrane. The phospholipids include molecules like phosphatidylcholine, phosphatidylethanolamine, and phosphatidylinositol. Guess what unsaturated fatty acid is in each of those? That’s right: arachidonic acid.
So arachidonic acid isn’t evil, but rather, essential for life. How does this play into seed oils? Arachidonic acid is synthesized from linoleic acid, the main villain in the seed oil story. And because linoleic acid (an omega-6 fatty acid) is found in marginally higher levels in seed oils versus non-seed vegetable oils, the seed oils must be the culprit, right?
What they leave out is that arachidonic acid itself is found in dietary sources like meat, especially organ meats (sorry, Liver King), egg yolks, certain fishes, and foods made with animal fat.
Dietary linoleic acid is found in seed oils, but also found in nuts, seeds, and soy (tofu, anyone?). And, only about 0.2% of linoleic acid we ingest is actually converted into arachidonic acid.
Anyway, seed oils have been painted as this “inflammatory villain” for a long time, even though copious data demonstrate that consumption of seed oils, even specifically linoleic acid, are not implicated in any chronic diseases associated with inflammation. Many studies suggest that linoleic acid is protective against cardiovascular disease, is associated with improved physical function in older adults, and is linked to a 20% reduced risk of death.
This study makes observations about signaling molecules in tumor biopsies.
The group identified 211 different lipid products that seemed to be distributed differently in the tumor tissue samples versus the normal tissue. 211 different molecules across 5 different groups of lipids: fatty acyls, glycerolipids, glycerophospholipids, sphingolipids and sterols. That is a HUGE bucket of chemicals.
All these lipids play essential roles in our bodies, including in the context of cancer. Cancer is a diverse and complex class of diseases (discussed here), and part of their pathology involves creating an environment, the tumor microenvironment (TME).
The TME is a dense ecosystem of tumor cells, bystanders, immune cells, and more. These cells are in a dynamic interplay within this ecosystem, which includes methods to communicate with each other, through protein and lipid-based signals.

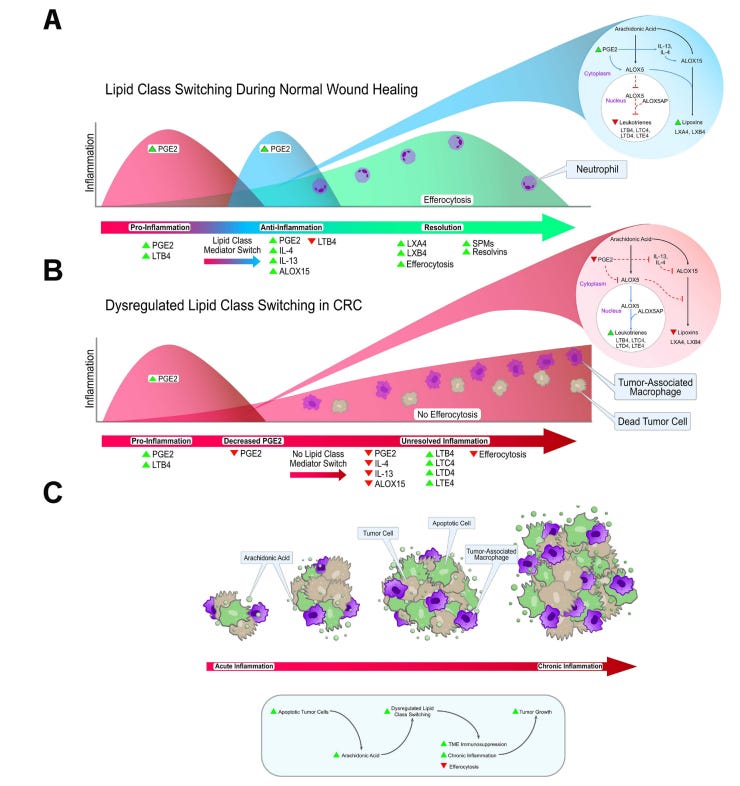
This study looked at lipid mediators already known to be involved in cellular processes, and based on patterns they observed, the team proposes a hypothetical scenario of what might be happening in CRC. They present that in a schematic:
But that’s all it is. This figure outlines what their next research steps might be, something all of us who have published biomedical research have done at some point. Schematics are very popular in academic publishing.
Essentially, this group thinks that some of these changes in lipid profiles - both increased gene expression and decreased gene expression in the CRC biopsies compared to the normal tissues - may have some role in immune cell function - and suggest that this might be a path to explore in the future.
The study doesn’t assess dietary intake of seed oils or ultraprocessed foods at all, much less how it might relate to colorectal cancer.
Not once in the study methods or procedures is dietary intake documented. So why are the media outlets and influencers saying this?
Well, they didn’t read the study. They definitely didn’t read the materials and methods. And they definitely didn’t understand the results.
It’s a very dense study with a lot of large data sets put together in data visualizations that are typical of spatial biology work. Even for someone like me who does this type of work on a regular basis, it takes some time to sift through.
Even though the study had zero relationship between these molecular analyses and diet, I found it bizarre that the senior author stipulates in an interview that he doesn’t think it’s “seed oils you cook with” but “seed oils in ultraprocessed food” could play a role
My guess? He knows seed oils have no evidence to support a role in cancer but also he wants this study to get more attention than the less sexy but more realistic summary that’s found in the actual paper.
I also found it interesting he talked about seed oils as a contributor to arachidonic acid, but not animal food sources that contain actual arachidonic acid - perhaps he has some person bias.
Either way, the study can’t speak to any role of either seed oils or processed foods - or animal food products. To date, studies claiming processed foods are related to cancers are association based only, and leave out key confounding variables - like the lack of fiber in a person’s overall diet - which is a known contributor to increased risk of colorectal cancer.
More on ultraprocessed foods below in a piece I wrote months back:
Fear-mongering about "processed foods" is harming public health and science literacy.
Yes, the media outlets are at it again, misleading and demonizing foods.
Colorectal cancer rates are not SKYROCKETING among young people.
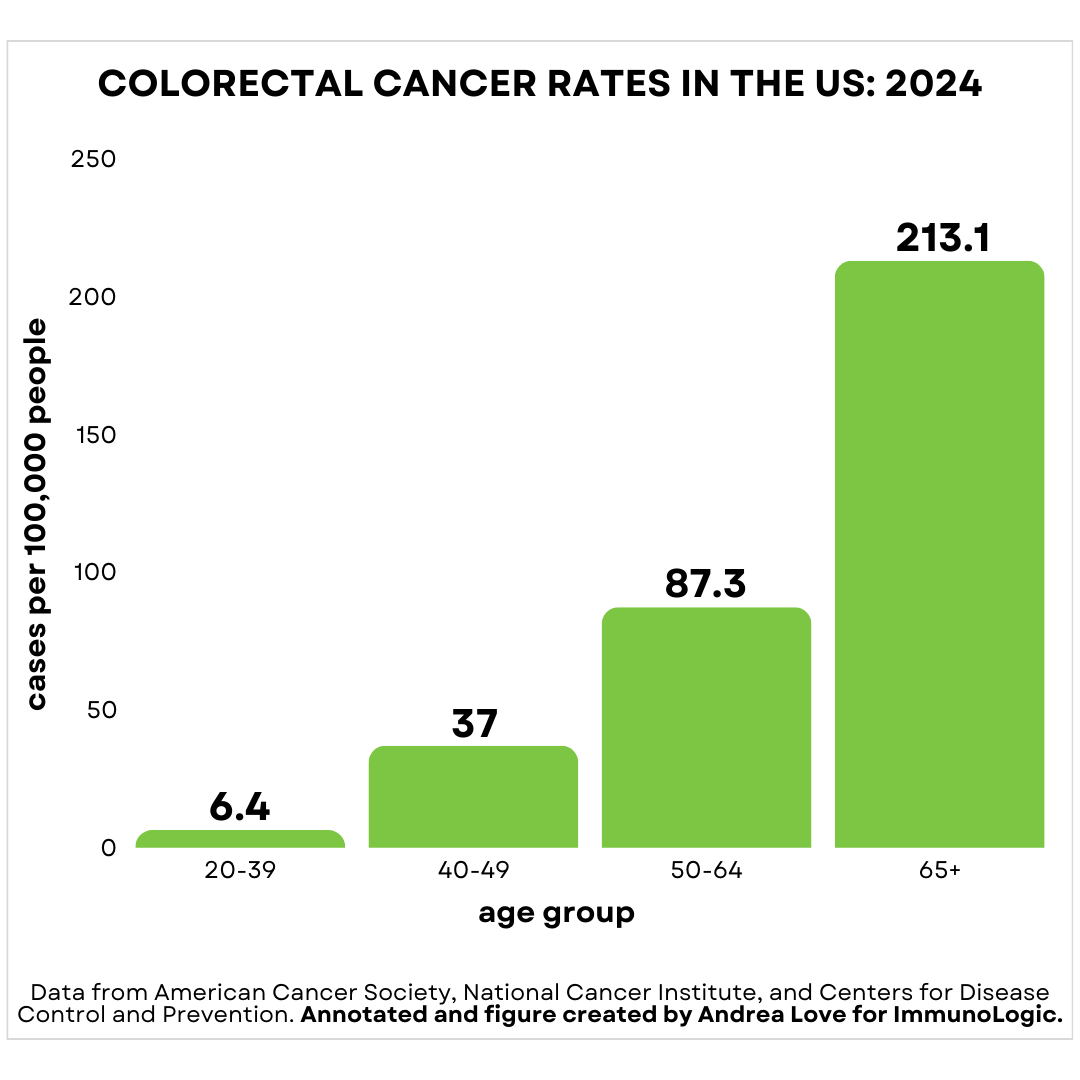
Colorectal cancer rates are the highest in adults over 65.
Colorectal cancer in adults 65 and older occurs at a rate of 213.1 cases per 100,000. In reality, adults 20-30 are the least common demographic to develop colorectal cancer.
There has been a modest increase in the rate of colorectal cancer among adults under 50, roughly 1-2% every year. On the flip side, colorectal cancer rates have decreased in adults over 50 by 1-2% ever year.
Among adults, the rate of colorectal cancer diagnoses are:
20-39: 6.4 cases/100,000
40-49: 37 cases/100,000
50-64: 87.3/100,000
65+: 213.1/100,000
When we say the rate has increased 1-2% every year, that is relative to the base rate. Among adults 20-39, case numbers would go from 6.4 per 100,000 to 6.464 cases per 100,000. For adults 40-49, a shift from 37 per 100,000 to 37.37 cases per 100,000.
There are 150,000 cases of CRC diagnosed every year. Based on the number of Americans under 50, that means an additional 216 cases of colorectal cancer will be diagnosed each year in adults under 50, a total of 21,927 cases.
The age-adjusted probability that someone under 50 will be diagnosed with colorectal cancer is 0.3%.
Sounds a lot less scary with context, right? And media outlets leave out the fact that we are now screening more adults under 50, because:
In 2021, the US Preventive Services Task Force (USPTF) changed the age for colonoscopy screening from 50 to 45.
In 2019, the FDA approval of the first non-invasive DNA-based test for colon cancer, Cologuard, was expanded to individuals 45-49.
So in the last 5 years, we have shifted the pool of adults that would receive routine colorectal cancer screening down 5 years. Remember: rate is a function of both ability to detect and diagnose AND actual occurrence of the disease.
We already know many risk factors for colorectal cancer.
Risk factors associated with early onset cancers, including colorectal cancers are:
Diets low in fiber & high in animal fats (spoiler: animal fats have arachidonic acid!)
Moderate and excess alcohol consumption
Tobacco and non-tobacco smoking products
Sedentary lifestyle.
Yes, many of the same risk factors that have long been associated with cancers.
Colorectal cancer isn’t coming for everyone under 50.
And it isn’t caused by seed oils, no matter what a chiropractor tells you. But cancer disinformation is a public health threat. Endorsing, elevating, and legitimizing falsehoods is harmful. Collective effort is needed to combat it. In the case of cancer, truth is a matter of life and death.
Thank you for supporting evidence-based science communication. With outbreaks of preventable diseases, refusal of evidence-based medical interventions, propagation of pseudoscience by prominent public “personalities”, it’s needed now more than ever.
Facts matter,
Andrea
“ImmunoLogic” is written by Dr. Andrea Love, PhD - immunologist and microbiologist. She works full-time in life sciences biotech and has had a lifelong passion for closing the science literacy gap and combating pseudoscience and health misinformation as far back as her childhood. This newsletter and her science communication organization are born from that passion. Follow on Instagram, Threads, Twitter, and Facebook, or support the newsletter by subscribing below:







My mother saw headlines about this and started questioning whether she should be using the grapeseed oil in her pantry. I hadn't heard about it yet (because I screen my news sources) but immediately had my doubts because I follow the commentary like yours on the "alt-health" movement. Even more so when I found who was publishing the fear mongering headlines.
She's science literate enough to understand once I explained what the study was actually about. We had a discussion about why seed oils are a hot topic right now and why is important to pay close attention to who is publishing the headlines that randomly pop up on your phone. I wish she would just turn those off. But it's so easy to see how this misinfo spreads when people don't look much past the headlines or don't have a biologist in the family that they trust and listen to about this stuff.
I agree that claiming seedoils are causing cancer in a headline out strips the data. But why do you claim they do NOT cause cancer in your headline? Surely that out strips the data as well.
" the study didn’t look at any sort of dietary contributors in the context of colorectal cancer". So doctor, where is your study showing it does NOT cause cancer?