Cancer: hundreds of complex diseases that are plagued with misinformation
Lack of understanding of cancer underlies harmful pseudoscience that circulates rampantly
Cancer is a commonly misunderstood class of diseases.
Cancer. A term that connotes fear and anxiety to almost everyone. And of course, why wouldn’t it? Cancer is the second leading cause of death in the US, trailing heart disease. What many people don’t realize though is that cancer is a huge bucket of different diseases; there isn’t just one CANCER. And all cancers are incredibly complex diseases influenced by many factors, each unique to a given individual who has cancer.
And the reasons cancer is a leading cause of death today is because we are no longer dying of acute causes:
💉 Vaccine-preventable & acute illnesses
🤕 Surgical & wound infections
🦠 Foodborne & waterborne diseases
🩼 Trauma and injuries
🩻 Medical procedure complications
Which were the leading causes of death in the 1800s and even early- to mid-1900s. And it wasn’t like cancer didn’t exist: we just didn’t have tools to appropriately diagnose many cancers, understand which type of cancer, and treat them, so causes of death were often nebulous, or related to the most acute symptoms: organ failure, respiratory arrest, stroke, when in reality, these acute symptoms were the result of cancer.
Cancer is a catch-all for hundreds of different diseases.
There are nearly 200 different *types* of cancers currently categorized. Broadly speaking, cancer occurs when our own cells grow uncontrollably and no longer listen to all of the regulatory processes our body has. Every single person who develops cancer has a uniquely distinct cancer, because we are all genetically distinct from each other, so when we say types, we are referring to classes or categories of cancers. But in reality, every single cancer is unique. One person’s breast cancer is not identical to another person’s breast cancer. And this underscores why there is not, and will never be, a universal cancer treatment (more on that to come).
Cancers all share certain hallmarks.
Cancer cells become de-differentiated, meaning they lose some of their characteristics of the cell type they originated from. When cells become lineage-committed, they have finite life spans and functions. In cancer, cells regress, which allows cancer cells to ignore many cues, extend their life span, and growth in places in the body they don’t belong. Cancer cells ignore signals that normally tell cells to stop dividing or that begin a process known as programmed cell death, or apoptosis, which the body uses to get rid of unneeded cells.
Cancer cells also influence normal cells, molecules, and blood vessels that surround and feed a tumor—an area known as the tumor microenvironment. Cancer cells can induce nearby normal cells to form blood vessels that supply tumors with oxygen and nutrients, which they need to grow. These blood vessels also remove waste products from tumors.
Cancer cells are also often able to evade the immune system, which normally identify cells that have abnormal structures or functions and flag them for destruction. Cancer cells are antigenic, meaning that they express antigens that the immune system recognizes as hostile. Just like the patrolling for foreign invaders, our immune system is critical for seeking and destroying our “self” cells that are no longer behaving as they should. Unfortunately, cancer can also exploit this. Some cancer cells are able to “hide” from the immune system through a variety of mechanisms, which allows them to evade these surveillance and control processes the immune system uses to keep any abnormal cells from growing into cancer (we will discuss this more in the future).

Cancers are diseases of accumulated mutations. There is no single cause of cancer.
Cancers occur when our normal, healthy cells start to grow out of control and no longer listen to cues and signals to stop growing. Cancers are hundreds of different illnesses that result from abnormal cellular processes such as uncontrolled cell growth and division.
Cells have defined lifespans - certain cell types have different life spans than others. When they’ve reached the end they die and new ones divide to replace them. In cancer this orderly process breaks down as a result of mutations. As cells become more and more abnormal, old or damaged cells survive when they should die, and new cells form when they are not needed. These extra cells divide without stopping and form growths called tumors. These mutations and abnormal processes progress over someone’s life, which is why the median age of cancer incidence is 60 years old.
Cells no longer listen to these cues as a result of accumulation of certain mutations. Remember, mutations are random errors that occur in an organisms DNA, most often when cells are reproducing (through mitosis or meiosis). Currently, there are over 400 different genes that have been linked to cancer progression. Of course, not all of them are involved in each cancer, and some genes play a much larger role than others.
Genes that are directly linked to cancer are those that are involved in correcting these random errors in DNA or regulating cell growth and division:
DNA Repair Enzymes
Tumor Suppressor Genes
Oncogenes
DNA Repair Enzymes directly correct errors in DNA that occur.
The good news is that humans have a lot of ways to proofread DNA and correct those errors: these are DNA repair mechanisms. Every cell in our body surveilles itself and ensures errors aren’t passed down to daughter cells.
Depending on the type of DNA damage, different repair processes are implemented, which are facilitated by enzymes that cut out or replace the incorrect portion of DNA. However, if the genes for those DNA repair enzymes themselves become mutated, those error-correcting processes may no longer work.
Normally, these genes (and the proteins they produce) ensure that no mistakes are made when DNA is copied from old to new cells during normal replication. However, if they are mutated themselves, they can miss mistakes when DNA is copied & introduce mutations in genes that control cell growth.
BRCA1 & BRCA2 are DNA repair genes. Inherited mutation in one of them increases risk for breast, ovarian as well as prostate cancer.
Tumor suppressor genes restrict uncontrolled growth of cells and suppress tumor formation.
When tumor suppressor genes are functioning, they help prevent tumor development by deciding whether a cell will divide or self-destruct through processes such as apoptosis if the cell no longer looks and behaves normally. If the tumor suppressor gene itself is mutated, the tumor suppressor function can be inhibited, allowing for abnormal cells to grow and multiply.
TP53 is a critical tumor suppressor gene. It produces the protein p53 which has numerous roles in regulating cell cycle and growth checkpoints.

Oncogenes are mutated versions of proto-oncogenes that promote uncontrolled cell growth.
Normally, proto-oncogenes function are important to control cell growth, division, and facilitate cell survival. However, if a proto-oncogene becomes mutated, it may turn into an oncogene. Oncogenes are like a stuck gas pedal; they can cause normal cells to growth out of control, no longer listen to normal cell survival or cell death cues, and turn healthy tissue into cancer.
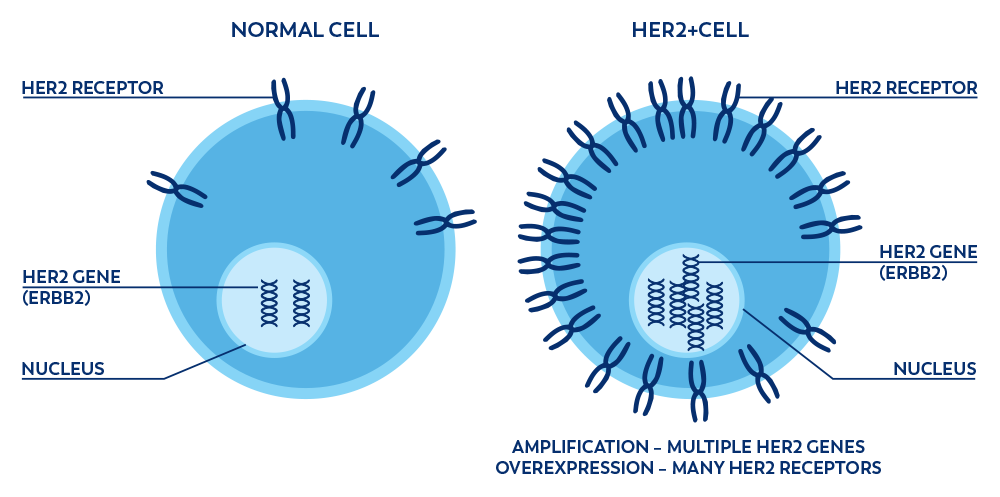
Sometimes, this is related to over-expression of the normal protein, where regular expression would lead to normal growth rates, but excessive expression leads to too much cell growth.
HER2 is an oncogene which is overexpressed. Too many copies of HER2 leads to too many HER2 proteins on the cell, leading to excessive cell growth. HER2 overexpression is present in about 20% of breast cancers, 20% of gastric cancers, and 5% of colorectal cancers.
Gene mutations can be inherited or occur over someone’s lifetime.
Inherited mutations are DNA mutations that are present in every cell of a person's body. These are called 'germline mutations' and they occur in sperm and/or egg cells, so are passed to a fetus during fertilization and conception. These inherited mutations are the mutations that result in cancers occurring among people at earlier ages, including in children.
Acquired mutations are DNA mutations that occur over the course of a person’s lifetime. Acquired mutations are not present in sperm or egg cells, and often are only found in certain cell types. These are not passed to children. 80% of DNA mutations that lead to cancer are acquired mutations. These mutations typically increase over the course of someone’s life, which is why most cancers appear later in life.
Not all gene mutations lead to cancer.
A common misconception is that cancer is a single cause. In reality, cancer is what we call a multifactorial disease: many things contribute to the development and progression of cancer. Mutations that help abnormal cells evade self-destruction cues may allow them to grow and multiply to form a cluster of cells. We often refer to this as a tumor (blood cancers are often referred to as liquid tumors).
Cancerous tumors are malignant, which means they can spread into, or invade, nearby tissues. In addition, as these tumors grow, some cancer cells can break off and travel to distant places in the body through the blood or the lymph system and form new tumors far from the original tumor, a process called metastases. Cancers often start as localized, and can then spread locally or further throughout the body. The degree to which cancer has spread from the originating location feeds into how a cancer would be staged by a clinician.
Unlike malignant tumors, benign tumors do not spread into, or invade, nearby tissues. Benign tumors can sometimes be quite large, but generally don’t have as many risks as cancer does. When removed, they usually don’t grow back, whereas malignant tumors sometimes do. Unlike most benign tumors elsewhere in the body, benign brain tumors can be life threatening (due to the location of the tumor).
Cancer cells differ from normal cells in many ways that allow them to grow out of control and become invasive. One important difference is that cancer cells are less specialized than normal cells. That is, whereas normal cells mature into very distinct cell types with specific functions, cancer cells do not. This is one reason that, unlike normal cells, cancer cells continue to divide without stopping.
Cancers are categorized in several ways.
Type of tissue or cell affected
Type of organ affected
Type of mutation in the cancer
Stage of progression of the cancer
Some examples:
Carcinomas are cancers of epithelial cells. These are parsed further by certain types of epithelial cells, such as squamous cell carcinomas, cancers of squamous cells (special type of epithelial cell), or basal cell carcinomas, which are basal epithelial cells.
Sarcomas are cancers of bone or soft tissues (muscle, fat, blood vessels, lymph vessels, and fibrous tissue (such as tendons and ligaments). Parsed further, osteosarcomas are the most common type of bone cancer. Kaposi sarcomas are cancers of the skin, lymph nodes, lining of the mouth, nose, and throat, and other tissues.
Leukemias are cancers of the leukocytes, our white blood cells (sometimes other blood cells). Leukemias are not solid tumors, but rather circulating cancers in our blood (we often called these hematologic malignancies, or cancers of the blood). There are many different types of leukemias, as they can be further classified by the white blood cell type impacted and the rate of the disease progression.
For example, acute myelogenous leukemia (AML) is characterized by rapid onset impacting myeloid cells (cells that would become granulocytes, red blood cells, or platelets (see this post where I discussed the immune cell lineages).
Chronic lymphocytic leukemia (CLL) as another example is associated with slower disease progression. It is the most common cause of leukemia among adult, with onset occurring in middle age, and impacts the lymphocytes (B cells and T cells).
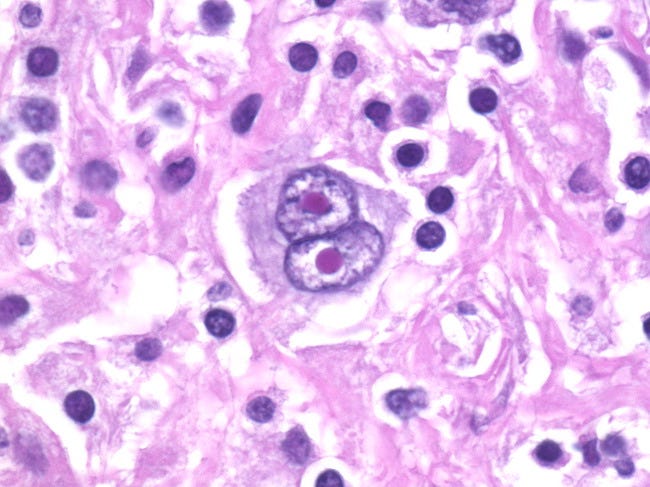
Lymphomas are cancers of lymphocytes specifically (T and B cells): mainly Hodgkin and non-Hodgkin lymphomas, both of which are further divided. However, if a specific type of cancer cell called a Reed-Sternberg cell is presented, the lymphoma would be classified as Hodgkin’s lymphoma. If not, then it would be non-Hodgkin’s. Reed-Sternberg cells only account for 1% of cancerous cells in Hodgkin’s lymphoma, but are large, often multinucleated giant tumor cells.
Multiple Myelomas are plasma cell cancers. Plasma cells are specialized B cells that produce antibodies. In multiple myeloma, these plasma cells grow out of control, no longer produce antibodies (which help to fight off invading pathogens and perform other functions), and out-compete our normal immune cells.
Melanomas are cancers that occur in our melanocytes, which are specialized pigment cells found in our skin.
Central nervous system cancers are similarly named for the cells they originate in. Gliomas originate from glial cells, meningiomas from the meninges, astrocytoma from astrocytes, etc.
And of course, there are other types of cancers such as germ cell tumors and endocrine tumors that have specific naming systems.
Risk factors include genetic and lifestyle influences.
Rough estimates suggest that 30-50% of all cancers are preventable as they are linked to modifiable risk factors. A non-exhaustive list is below. It is also important to note that simply engaging in some of these behaviors does not guarantee you will develop cancer, and on the converse, having the most healthy lifestyle does not guarantee you won’t develop cancer. Many things are out of our control.
Unfortunately, the collective fear of cancer is exploited by misinformation.
I hope this piece makes it clear that cancer is incredibly complex and too often, fear-based messaging about what causes cancer or what “cures” or prevents cancer are not based in reality. The fear of cancer is exploited by broad gaps in understanding of cancer and complexities of the diseases. The tactics are effective because - of course - nearly everyone knows someone who has cancer, who died from cancer, or who is in remission from cancer. No one wants to hear that word as it relates to their own health. But understanding of cancers and how they develop will empower you to better navigate the misinformation and pseudoscience about topics related to cancer, of which we will discuss many in the future!
Thanks for joining in the fight for science!
Thank you for supporting evidence-based science communication. With outbreaks of preventable diseases, refusal of evidence-based medical interventions, propagation of pseudoscience by prominent public “personalities”, it’s needed now more than ever.
Your local immunologist,
Andrea







Great explanation of what “cancer” is and means. In addition to many cancers not being diagnosed in the past, there was also shame in talking about cancer. My great-grandmother died from breast cancer in the 1930s. The family told people a horse bit her. She died at home when my grandpa was still a kid. His dad would take the kids to the tavern to get a break from hearing their mom in pain because all they had to give her was aspirin. So many back-in-the-day stories I grew up hearing from older generations sounded horribly hard and sad. Thanks for sharing this perspective.