Are cancer rates skyrocketing? No, not really.
Cancer rates depend on how well we can detect and diagnose cancers. Clickbait headlines mislead you about this complex category of diseases.
Cancer is widely misunderstood by most people.
If you talk to anyone, they would know the term cancer. Most people know someone who was diagnosed with cancer: roughly 1 in 3 people will be diagnosed with cancer at some point in their life. Cancer is a huge bucket of hundreds of unique diseases that are widely misunderstood.
There are a few reasons for this misunderstanding:
Cancers are incredibly complex diseases that are influenced by many factors.
Intentional misinformation spread online is designed to spread fear and target people who are navigating cancer.
Fear and stigma about cancer, particularly about death due to cancer.
Our understanding of cancers is growing every day, meaning knowledge about diagnosing, treating, and prevention evolves.
Media outlets frequently oversimplify and misrepresent topics related to cancer.
Healthcare providers that aren’t qualified to speak on cancer frequently mischaracterize the biology and current data.
And unfortunately, recent headlines and stories about “rising cancer rates” have gone viral because of all of these reasons. So let’s talk about it.
Americans are no longer dying of acute causes.
Today in the US, cancer is the second leading cause of death behind heart disease. That’s because we are no longer dying at younger ages as a result of acute causes:
Vaccine-preventable & acute illnesses
Surgical & wound infections
Foodborne & waterborne diseases
Trauma and injuries
Medical procedure complications
This is a good thing! Scientific knowledge and medical interventions that utilize that knowledge improve the quality and quantity of our lives.
Vaccines, water treatment, antibiotics, disinfectants, medical device development, sterilization technologies, food preservation methods… all of these technologies were created through science.
As a result, our life expectancy has increased. In 1900, our life expectancy was below 50 years old. Today, average life expectancy is 73.5 (men) and 79.3 (women) in the US.
US life expectancy trails other developed nations such as Canada (82.3), Australia (83.2), Japan (84.7), Switzerland (83.5), UK (81.2), and France (82.7), as a result of health disparities and social determinants of health due to lack of a national healthcare system.
Acute causes of death are still very much a concern in underserved and developing nations, where water sanitation, foodborne illness, and infectious diseases are significant health threats. For purposes of this piece, I am going to focus on US data.
Increased life expectancy means people die from diseases of aging.
Since we aren’t dying [as often] from acute causes at younger ages, we are living to where cancers may become a health issue. Cancers, broadly, are diseases of aging.
80% of cancers occur in individuals over the age of 50, and the median age of cancer diagnosis is 61 years.
Cancers occur when our cells stop behaving normally. This happens when genes that are required to regulate cellular processes become mutated. Gene mutations occur randomly as a result of errors during DNA replication. The more cell divisions, the higher the likelihood of an error occurring, leading to a mutation.
Our body is pretty good at repairing these errors. But, eventually, some of these errors might stick, leading to gene mutations, uncontrolled cell growth, and cancer. (Read my skin cancer piece, below, for more)
Yes, there are cancers linked to inherited gene mutations that can cause pediatric cancers and cancers at younger ages. Broadly speaking though, cancers take time to progress. Things that occur over the course of your life contribute to that potential progression.
All cancers are not equal. That means cancer trends can’t be lumped into one category.
Too often, I read headlines like “cancer rates are skyrocketing among young people” or “cancer rates are climbing” or “rising rate of young people getting cancer” and aside from these being misleading, they’re not actually accurate.
Cancers are hundreds of diseases, categorized by multiple different criteria:
The cell type they originate from (e.g. carcinoma vs. sarcoma vs. leukemia vs. lymphoma vs. meningiomas)
The tissue type they originate in (e.g. lung vs. skin vs. breast vs. oropharyngeal vs. colorectal vs. cervical)
Specific gene mutations in the cancer (HER2-positive vs. BRCA1 185delAG vs. triple negative vs. BRAF V600E)
The degree of spread of the cancer (TNM classifications followed by staging [0-4])
Even “identical” types of cancers differ person to person. If you had a group of patients all with stage 2 HER2-positive invasive ductal carcinoma (invasive breast cancer derived from epithelial cells in milk ducts), each cancer would STILL be different. Cancers originate from your cells - and every person is genetically unique.
You can’t lump [CANCER] into a single category when looking at trends. You have to, at a minimum, parse by types of cancer. Often, we do this by tissue or cell type.
Cancer rates depends on how well we can diagnose cancers.
Cancer rates actually refer to cancer diagnoses, the ability to accurately detect the presence of cancer. Before anyone says otherwise, cancer has always been around - just because we didn’t have a name for it, doesn’t mean people weren’t developing cancers.
The inability to detect and diagnose cancer doesn’t mean it didn’t exist. Many cancers are diagnosed based on scientific tools that didn’t exist until recently.
Lower life expectancy meant that people were dying of other things before cancer had a chance to progress and be the ultimate cause of death.
Some cancer rates might appear to increase because we can detect them better, not because the cancer itself is occurring more frequently.
If we detect cancers at an earlier stage, they are more treatable, the likelihood of remission is greater, and prognosis is improved.
Our ability to detect breast cancers, especially early stage breast cancers, using mammography wasn’t possible until the 1960s. It was officially recommended as a cancer screening tool in 1976, and evolved further with the development of digital mammography in the 1990s.
What do you think happened between 1976 and 2000? Yep, breast cancer rates rose dramatically.
This wasn’t because more people were developing breast cancer, but because mammography meant earlier stage breast cancers could now be detected.
Ductal carcinoma in situ (DCIS), a non-invasive breast cancer that originates in epithelial cells in milk ducts, is considered the earliest stage of breast cancer. Between 1973 and 1992, DCIS diagnoses rose by over 300%. Similarly, rates of stage 1 breast cancers among women 40 and older increased from 82 per 100,000 in 1975 to over 200 per 100,000.
Man, imagine if social media existed back then? Whew, the clickbait we’d have to debunk!
Breast cancer rates have decreased an average of 0.3% annually since the 1990s.
Health outcomes related to cancers are improving.
We are able to diagnose, characterize, and treat cancers at earlier stages before the disease becomes more serious and less manageable. In 1950, 31.9 deaths due to breast cancer occurred per 100,000 individuals. Today, the death rate is 19.4 per 100,000.
Improved mortality is also attributed to better treatments. If we can detect cancers earlier, before they invade lymph nodes, compromise the immune system, and spread into other organs, they are better able to be treated, which means people will survive more. Breast cancer mortality declined by 58% reduction between 1975 and 2019 as a result of improved detection and treatment.
Cancer-related mortality rates have improved for many cancer types.
Every day, we have more treatment options for even more aggressive and less common cancers. Combination therapies coupling immunotherapies, surgical interventions, cell and gene therapies, and even traditional chemotherapeutics and radiation-based treatments improve quantity and quality of life after cancer diagnosis.
Surprise! Many cancer rates are declining.
Unfortunately, you won’t hear headlines extolling this, but we’ve made a lot of progress when it comes to certain types of cancers, and the reality is, there are lots of cancers that are decreasing in prevalence.
As noted, breast cancer rates have been declining since the 1990s.
Cervical cancer rates have declined dramatically as we have been able to prevent HPV infections, which cause over 90% of cervical cancer cases. That’s right, vaccines prevent cancers. Read my piece below for more.
Lung cancer rates have declined 23.35% between 1990 and 2019 as smoking, the biggest modifiable risk factor, has declined. Lung cancer rates dropped to 49.1 cases per 100,000 in 2021 compared to 70.7 cases per 100,000 in 1999.
Other declining cancers include prostate, stomach, Hodgkin lymphoma, bladder, laryngeal, and even colorectal cancer in individuals 50 and older.
Which brings me to the next point:
Irresponsible and reckless reporting causes exaggerated fears about cancer and adds to spread of disinformation.
I’m sure you’ve seen headlines like “colorectal cancer surging among young people”
or “millennials are at higher risk of cancer than older generations” with imagery designed to scare you.
These headlines are designed to be clickbait, but they don’t tell the full story.
The phrase “young” here, this refers to adults under 50 years old. Since colorectal cancer has been all over the news recently, what’s real when it comes to colorectal cancer in “young” adults?
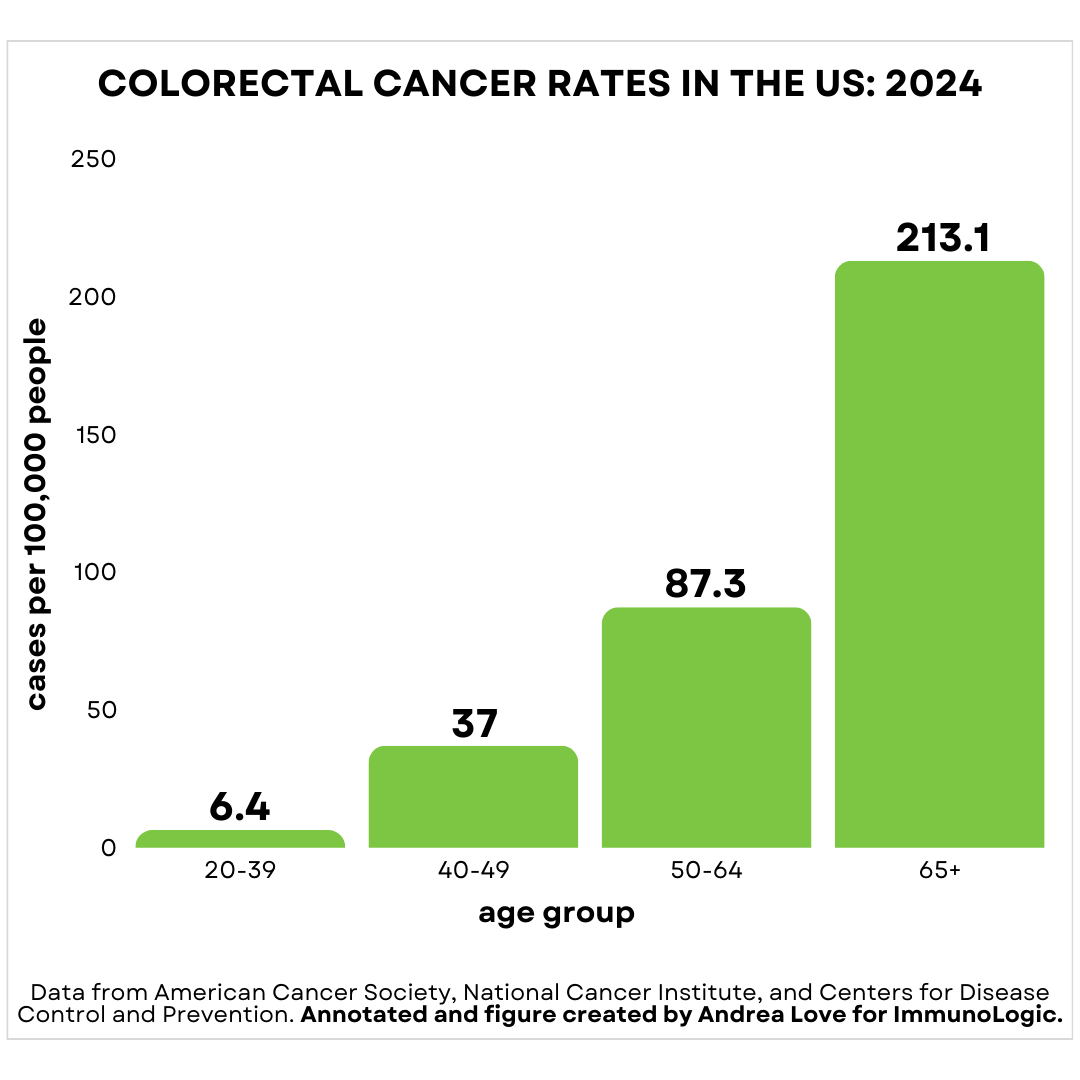
Colorectal cancer rates are the highest in adults over 65.
Colorectal cancer in adults 65 and older occurs at a rate of 213.1 cases per 100,000. In reality, adults 20-30 are the least common demographic to develop colorectal cancer.
There has been a modest increase in the rate of colorectal cancer among adults under 50, roughly 1-2% every year. On the flip side, colorectal cancer rates have decreased in adults over 50 by 1-2% ever year.
Of course, the media headlines only talk about the first half.
But let’s look at some more numbers.
Among adults, the rate of colorectal cancer diagnoses are:
20-39: 6.4 cases/100,000
40-49: 37 cases/100,000
50-64: 87.3/100,000
65+: 213.1/100,000
The risk of colorectal cancer is orders of magnitude higher as you age.
What about rates increasing among adults under 50?
When someone says the rate has increased 1-2% every year, that is relative to the case rate. That means among adults 20-39, case numbers are going from 6.4 per 100,000 to 6.464 cases per 100,000. For adults 40-49, that’s a shift from 37 per 100,000 to 37.37 cases per 100,000.
There are roughly 150,000 cases of colorectal cancer diagnosed in the US every year.
There are 86 million Americans aged 20-39. A increase of 1% of the rate means going from 5,505 cases per year to 5,559 cases of colorectal cancer per year.
There are 43.8 million Americans aged 40-49. An increase of 1% of the rate means going from 16,206 to 16,368 cases of colorectal cancer per year.
So while there is a slight increase in number of diagnosed cases of colorectal cancer, but it is not the panic-inducing scenario social media, media outlets, and online influencers would have you believe.
Media outlets often cherry-pick case reports to make it seem that early onset cancers are more common than they are.
This leads people to think that these outlier cases among younger adults are the norm, when in fact, they are the exception.
In addition, media outlets frequently use inappropriate “experts” as sources. I saw a media outlet interview a psychiatrist about colorectal cancer causes. If it weren’t obvious, a psychiatrist is a medical provider that doesn’t have expertise in relevant fields. If they lack the deep knowledge on this topic, it means they are more likely to share misinformation. Even if they are well-intentioned, their authority gives that misinformation legitimacy, which only fuels the pseudoscience fire.
Increased rate of colorectal cancer also relates to changes in screening recommendations.
In 2021, the US Preventive Services Task Force (USPTF) changed the age for colonoscopy screening from 50 to 45, which means colorectal cancer cases in adults under 50 will be captured than were previously. Additionally, the first non-invasive DNA-based test for colon cancer, Cologuard, was approved in 2014, which further expands the pool of individuals getting screening tests for colorectal cancers. In 2019, the FDA approval was expanded to individuals 45-49.
So when headlines say that “young people” account for ~20% of colorectal cancer cases, that is pretty much the same story: young people refers to those under 50.
What should we be concerned about with regard to colorectal cancers?
Risk factors associated with early onset cancers, including colorectal cancers are diets low in fiber and high in animal fats (CarnivoreMD, you hear that?), alcohol consumption, tobacco and non-tobacco smoking products, and a sedentary lifestyle. Yes, these are many of the same risk factors historically associated with cancers.
Should millennials and Gen Xers be panicked about cancer risks? No.
Headlines suggesting that millennials and Gen Xers are at higher risk of cancer than Boomers are a manipulation of cohort-based epidemiological data. Let’s quickly tease this apart. Remember: 80% of cancer diagnoses occur in individuals 50 and older and median diagnosis age is 61.
This study compared incidence for 34 cancer types between 2000 and 2019, based on birth year, to make conclusions about cancer risk between generations, including Boomers (b. 1946 - 1964), Gen X (b. 1965 - 1980) and Millennials (b. 1981 - 1996).
The youngest Boomers, born in 1964, would have been 36 in 2000, and 55 in 2019. The oldest Boomers, born in 1946, would have been 54 in 2000 and 73 in 2019. This means that many of this demographic were possibly diagnosed with cancer before this data set. Those cases would not be included as cancer diagnoses in these data, thereby potentially skewing the data.
In contrast, Gen X would be hitting that age range during the data collection window. Gen X born in 1965 would be 35 in 2000 and 54 in 2019. This, plus adjusted detection guidelines and improved screening tools for many cancer types, means that you cannot simply compare cancer diagnosis rates apples to apples between these groups.
Collective fear of cancer is exploited by misinformation.
Cancer is incredibly complex and fear-based messaging about cancer prevalence, causes of cancers, and “cures” frequently mischaracterize data, manipulate information, or outright fabricate claims. Understanding what’s real and what’s not will help you navigate the rampant and lucrative world of cancer misinformation and pseudoscience that is designed to prey on your fear and vulnerability.
Thank you for supporting evidence-based science communication. With outbreaks of preventable diseases, refusal of evidence-based medical interventions, propagation of pseudoscience by prominent public “personalities”, it’s needed now more than ever.
Stay skeptical,
Andrea
“ImmunoLogic” is written by Dr. Andrea Love, PhD - immunologist and microbiologist. She works full-time in life sciences biotech and has had a lifelong passion for closing the science literacy gap and combating pseudoscience and health misinformation as far back as her childhood. This newsletter and her science communication on her social media pages are born from that passion. Follow on Instagram, Threads, Twitter, and Facebook, or support the newsletter by subscribing below:











Thank you once again.
My pet- phrase at work & of late on-line is 'context' which you consistently do. 🙂
I was very scared by these stories in the news, colorectal cancer is a big fear of mine. I’m grateful that you wrote this, thank you!