Mammograms do not cause cancer - and more breast cancer truths.
Misinformation spread by wellness influencers and unqualified celebrities undermine critically important science and health interventions
October is Breast Cancer Awareness Month and cancer misinformation is rampant as always. Recently, I wrote about the harms of celebrities like Elle MacPherson claiming - to the entire world - that they cured their cancer with alternative treatments while omitting that they actually got conventional treatments. In Elle’s case, she had a lumpectomy, standard of care for early stage breast cancer.
Endorsing "alternative" cancer treatments is a danger to public health
I’ve been wanting to start to dig into cancer pseudoscience for a long time, and in my other pieces, I’ve really only scratched the surface. But with the rampant headlines about Elle MacPherson, now is the perfect time to really start to get into it.
But her story is not the only example of hyperbole, pseudoscience, and disinformation spreading about breast cancer. And the issue is: these falsehoods cause serious harms.
So as we close out Breast Cancer Awareness Month, let’s tackle some of the most harmful myths: claims that cause people to forgo proven screening methods, not maintain lifestyle habits that reduce risk of cancer, and buy into unproven methods that do not treat or cure cancer, and can cause early death.
Cancer misinformation costs people their lives.
(some of this content previously appeared in my article for PopSugar, here)
Recently, another celebrity, Ananda Lewis, announced that she refused mammograms for years because she was told they were harmful. When she was diagnosed with breast cancer at stage 3, she also refused proven treatments. Now, her cancer is stage 4 and is considered incurable.
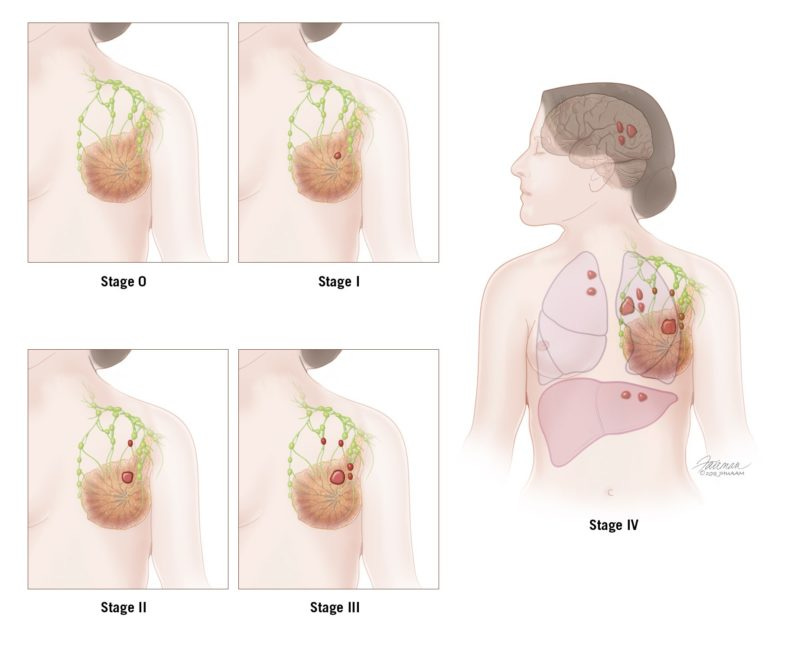
Stage 4, or metastatic, breast cancer is when cancer has spread beyond the breast and nearby lymph nodes and established tumors in other body sites: often bones, liver, lungs, and brain. Once cancer is this widespread in so many organs and tissues, it is nearly impossible to eliminate it.
Stage 4 treatments aim to minimize further spread, manage symptoms, and improve quality of life. Unfortunately, 5-year survival rates for stage 4 breast cancer is 25-30%. That means only 25-30% of these patients live for 5 additional year.
This is heartbreaking, more so because this likely could have been prevented.
Ananda was diagnosed at stage 3. There are 3 types of stage 3 breast cancer, stage 3A, 3B, and 3C, which relate to the size of the tumor and the number of lymph nodes that are involved.
The average 5-year survival of stage 3 breast cancer is about 72% (without knowing the specific staging). By forgoing proven treatments, Ananda has a 2.68-times higher chance of dying in the next 5 years.
The reason she opted out of evidence-based treatment? Because she was exposed to misinformation. If Ananda hadn’t been exposed to misinformation about treatments, she might have opted for things with evidence, instead of “detoxes”, diets, and supplements.
Mammograms and radiation from them DO NOT cause breast cancer.
If Ananda hadn’t been exposed to misinformation that mammograms were harmful, she might have gotten routine screening as recommended, which would have diagnosed her cancer earlier, when it could be treated with less invasive procedures and lower risk of recurrence.
This is an unfortunate story that we can use as a teachable moment:
Mammograms do use x-ray radiation, but the dose is tiny.
Let’s quickly refresh on the electromagnetic spectrum (I discuss this in the context of skin cancer here). X-ray radiation is ionizing radiation, which can cause DNA and cellular damage - depending on the dose and exposure. Our bodies have damage repair mechanisms that proofread and correct potential damage that can lead to mutations. When X-ray exposure is minimal, there is no marked increased risk.
The dose of radiation you are exposed to during a mammogram is miniscule.
A mammogram uses 0.4 millisieverts (mSv) of radiation. You're exposed to 10 times that level every year of your life simply by living on Earth. A flight from New York to California comes with 10 percent of the amount of radiation exposure you get during a mammogram. (Frequent fliers also need not be concerned.)
When we look at risk of x-ray radiation, we look at cumulative exposures. Low dose exposure typically falls below 100 mSv lifetime exposure. Below this level, there is minimal impact to cancer risk - and this is the category that most people fall into.
So let’s do some math based on the USPTF mammogram guidelines: every 2 years from age 40 to 74, which would be 17 mammograms, at a total of 6.8 mSv of radiation over the course of your life from mammograms.
The estimated added cancer risk is less that 0.01%, so you don’t need to be concerned that mammograms are potentially harming your health.
Not only do regular mammograms not contribute to breast cancer, but their role in screening for breast cancer is huge. Mammograms are the best early detection method and drastically improve survival.
Health outcomes related to breast cancers are improving.
Since we can diagnose, characterize, and treat breast cancers at earlier stages before the disease becomes more serious and less manageable, our survival and outcomes are improving. In 1950, 31.9 deaths due to breast cancer occurred per 100,000 individuals. Today, the death rate is 19.4 per 100,000. This is because of early interventions like mammograms.
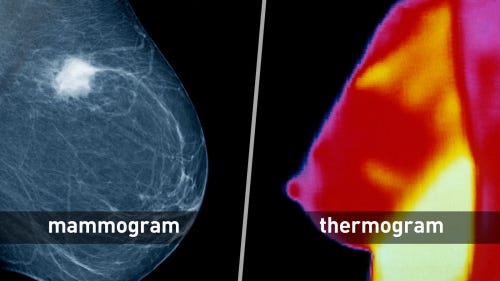
Don't opt out of mammograms or seek unproven alternatives like thermography.
Thermography is NOT an alternative to mammograms.
Thermography has gained legs in pop culture and wellness spheres. It is advertised by unqualified influencers, chiropractors, naturopaths, and others who claim that it’s a “safer” and “more accurate” method of detecting breast cancer than mammograms. This is false.
Thermography uses infrared imaging to detect heat signatures and patterns. Unqualified people who promote it claim that cancers “generate more heat” because of changes in blood flow and vasculature in tumors. There is not evidence to support this claim.
Thermography is not accurate for detecting cancers, breast or otherwise. It has low sensitivity - meaning it misses cancers that are present. It ALSO has low specificity - meaning it flags images that don’t have cancer. This means that it both under- and over-diagnoses cancers
There is no evidence to support the claims that thermography is even equivalent for early breast cancer detection. There are no largescale clinical trials to support its accuracy. There is no evidence that thermography results improve outcomes, and it certainly doesn’t detect cancers earlier than mammograms.
If you encounter someone recommended thermograms, steer clear.
Underwire bras don’t cause breast cancer.
Yet another pervasive myth which causes unfounded fears among too many people. This claim is based on the false notion that underwires - or tight fitting clothing - interfere with the circulation of the lymphatic system, causing toxins to build up in lymph nodes and breast tissue, which leads to cancer. There's no credible evidence behind this.
The idea of "toxins" accumulating in breast tissue is implausible based on how our bodies work. Your immune and lymphatic systems are complex and well-regulated; they are not impacted by wearing an underwire bra, even one that might be tight. There is no scientific basis to support this idea. All major and credible health organizations, including the American Cancer Society and the National Cancer Institute have concluded that there is no data that shows a link between bras (of any type) and an increased risk of breast cancer.
If you don’t want to wear a bra, do you. But don’t avoid bras because of this lie.
Antiperspirants ALSO don’t cause breast cancer.
I wrote about that myth in detail before, so just head here:
Aluminum-containing antiperspirants are safe and effective
Well, it’s sweaty season here in Philly so questions about antiperspirants are creeping up. There is an extensive market of “aluminum-free” deodorants and antiperspirants, as well as rampant claims on social media about the harms of aluminum-containing antiperspirants, so it’s time we set the record straight.
Sugar also doesn’t cause - or feed - breast cancer (or any cancers).
This belief stems from a feature of certain cancers, a phenomenon called the Warburg effect, where cancer cells consume glucose at a high rate due to metabolic demands. In fact, PET imaging (positron emission tomography) leverages this Warburg effect for cancer screening.
All cells need glucose to function, not just cancer cells. PET scans use a radioactive form of glucose that labels areas in the body that consume glucose quickly. This helps detect cancer cells, which will "light up" on a PET scan. But many healthy cell types also use glucose at high rates, and they light up on PET scans, too. The fact that PET scans use glucose doesn't mean eating sugar makes cancer cells grow faster. In reality, there is no direct link between eating sugar and cancer growth.
Sugar consumption is sometimes conflated with obesity, which is a risk factor for breast cancer, particularly after menopause. The goal should always be to eat a nutritious diet and maintain a healthy weight, but sugar itself also doesn't cause obesity. In fact, many foods that contain sugar are nutritious components of a healthy diet. You do not need to avoid sugar for fear of "feeding cancer."
I wrote about this one in much more detail here as well:
Sugar doesn't cause - or feed - cancer.
If you’re sensing a theme, you’re not wrong! Health misinformation frequently gains legs because someone misrepresents basic science principles, scientific data, or wildly extrapolates a phenomenon that exists, but not in the context it is misapplied.
Herbal and alternative remedies cannot cure or treat breast cancer.
Breast cancer is a scary diagnosis and the treatments can also sound scary. This causes some people to explore alternative options such as herbal remedies or supplements. But be aware, this can have serious consequences.
Opting out of proven treatments can increase risk of death.
If there were options out there that we knew worked, they would be incorporated into evidence-based treatment plans. For breast cancer, surgery, radiation, chemotherapy, and immunotherapies have proven to be effective treatments and cures.
Today, the vast majority of breast cancers are survivable if you seek proven treatments after early detection. The five-year survival rate is over 90 percent. But this isn’t the case if you opt for unproven alternatives. Five-year survival plummets to 58.1 percent and breast cancer patients have a 5.7-fold increased risk of death when using alternative treatments instead of proven methods.
More than that, patients who opt for alternative treatments are less likely to use conventional treatments in conjunction. They delay proven treatments until cancers progress to more severe disease, reducing treatment options. 34% of the alternative medicine group refused any sort of chemotherapeutic, compared to 3% of those receiving conventional treatments.
Anyone is at risk of breast cancer, so don’t forgo screenings just because you don’t have a family history.
Some people think that if they have no history of breast cancer in their family, they aren't at risk. This can create a false sense of security, and cause them to be less diligent about preventive breast cancer screenings or ignore symptoms or warning signs of breast cancers.
The reality? 80 to 85 percent of breast cancers occur in women with no known family history.
And: about 1% of breast cancers occur in men. While men often think they are exempt from this discussion, men do have mammary tissue and can, in less common instances, develop breast cancer.
While certain gene mutations like BRCA1 and BRCA2, genes that repair DNA damage, can increase the risk of developing some cancers (breast included), inherited mutations only account for 5-10 percent of breast cancers. Another 15-20 percent occur more often in certain families without known gene mutations, which is referred to as familial breast cancer.
The biggest risk factors for breast cancer are aging (true of all cancers), being female, and lifestyle factors (smoking, excess alcohol consumption, poor diet, inactivity). That's why awareness and routine screenings are important for everyone, regardless of family history.
Navigating breast cancer can feel daunting. It's worse when you're bombarded by misinformation and pseudoscience myths. Not only are these claims misleading, but they can prevent people from seeking appropriate diagnosis and treatment, and end up causing serious harm.
When it comes to breast cancer, many things are out of your control, but you can take some steps to reduce your risk. Early detection, a healthy lifestyle, and proven medical care are the best tools to prevent breast cancer. But fighting breast cancer is also about arming yourself with accurate information. Because when it comes to breast cancer, facts save lives.
Thank you for supporting evidence-based science communication. With outbreaks of preventable diseases, refusal of evidence-based medical interventions, propagation of pseudoscience by prominent public “personalities”, it’s needed now more than ever.
Stay skeptical,
Andrea
“ImmunoLogic” is written by Dr. Andrea Love, PhD - immunologist and microbiologist. She works full-time in life sciences biotech and has had a lifelong passion for closing the science literacy gap and combating pseudoscience and health misinformation as far back as her childhood. This newsletter and her science communication on her social media pages are born from that passion. Follow on Instagram, Threads, Twitter, and Facebook, or support the newsletter by subscribing below:







Thank you for your ongoing role in debunking garbage science. I’ll happily put on my underwire bra, apply antiperspirant and eat a cookie - all without fear. On a related note, is anyone else scared speechless at the thought of RFK Jr being in charge of the nation’s healthcare???