It's the sun, not sunscreen, that can cause skin cancers
Chemical AND mineral sunscreens are safe for use and help protect again skin cancer.
Did I think I would be writing a piece in 2024 to debunk claims that it’s sunscreens, not sun exposure, that contribute to skin cancer risk? No, I did not. Yet here we are.
Now, there will be a follow up piece on sunscreen and chemistry misinformation, but first, we have to discuss the factual reality that:
Ultraviolet (UV) radiation exposure from the sun is a modifiable risk factor for skin cancers.
Yes, there are people that vocally claim that sunscreen poses more of a risk for cancer than excess sun exposure. They’re wrong. It’s time we stop giving people room to spread harmful lies.
Several years ago, Andrew Huberman made up a study claiming sunscreen “toxins” were found in people’s brains. Now, he undermined an entire class of safe and effective sunscreens: chemical sunscreens. I guess we can give him credit that he finally acknowledged that UV exposure contributes to skin cancer?
Are people debating chemical sunscreen safety? Legitimate experts on the topic aren’t, but activist groups and unqualified people being perceived as experts might. And Huberman suggesting it’s a valid “debate” further legitimizes that. But this isn’t just about him.
I’ve seen countless accounts and media outlets circulating the same claims, undermining the safety of chemical sunscreens, and repeating the same unfounded statements. Even “scicomm” accounts that appeared during the pandemic are repeating the same misinformation about the purported higher risks of chemical sunscreens.
And let’s not mention that both classes of sunscreens ARE chemicals - a battle in branding that I won’t win, according to Dr. Michelle Wong, a legit expert in sunscreen and cosmetic chemistry. For scientific accuracy, chemical sunscreens are organic filters, and mineral sunscreens are inorganic filters.
Chemical AND mineral sunscreens are both safe for use.
Why do I care about this misinformation? Because many people don’t want to wear mineral sunscreens: the texture might be unpleasant and they cause white cast, especially on people with darker skin.
If people have been incorrectly led to believe chemical sunscreens are less safe and their *only* option are mineral sunscreens, they might not apply enough to provide adequate protection or they might not use it at all! If people are relying on false information and not using adequate protection against cancer, that’s a dangerous public health issue. Here’s the science.
Sunscreens help protect us and reduce the risk of skin cancers.
Ultraviolet radiation from the sun contributes to the development of skin cancers.
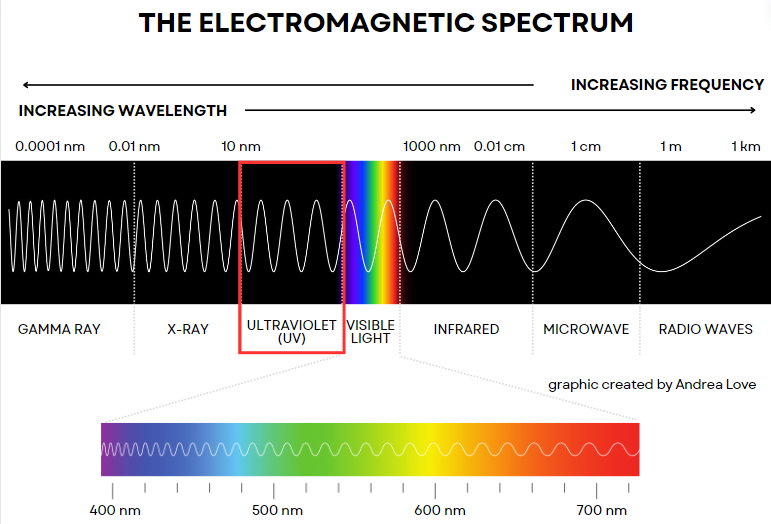
Let’s start with the electromagnetic spectrum: the range of all electromagnetic radiation sources. In layman’s terms, these are sources of energy that travel through space in waves. These include visible light - light humans can see, which we see as *white* but includes the colors of the rainbow (remember ROYGBIV?) when we separate individual wavelengths.
It includes longer wave energies like infrared, microwaves, and radio, and shorter wavelength energies like gamma radiation, x-rays, and ultraviolet (UV) (ultra- means beyond, so it’s energy just past violet in our visible detection range). Shorter wavelength energies have an increased frequency (the rate of the wave motion) and energy.
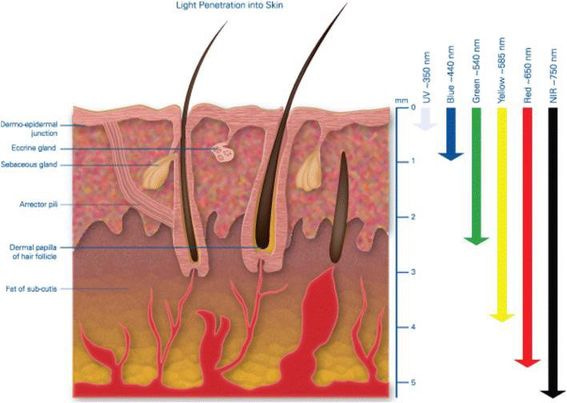
UV radiation from the sun has somewhat short wavelengths and intermediate energy, which means that it can penetrate into the skin, interact with different layers of the skin, and cause damage to molecules and cells within the layers of our skin.
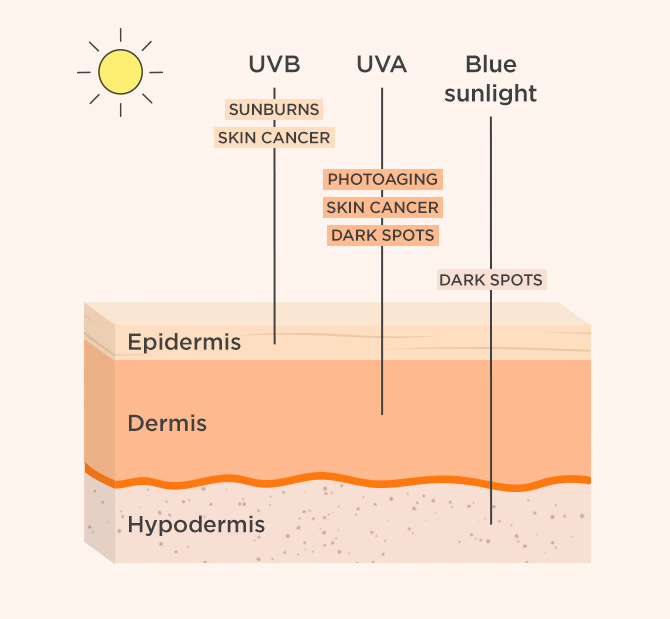
UV radiation from the sun contains UVA, UVB, and UVC. UVC is the highest energy UV but is absorbed by the ozone layer and does not get to Earth’s surface. Thus, we are mostly concerned with UVA and UVB as those are ones we are exposed to.
UVA and UVB radiation both contribute to skin damage caused by excess sun exposure.
UVB radiation has wavelength of 280-315 nm compared to UVA (315-400 nm), which means that UVB radiation has a shorter wavelength and higher energy compared to UVA. This energy, when it penetrates our skin, is absorbed by the tissues and transferred to molecules in our skin.
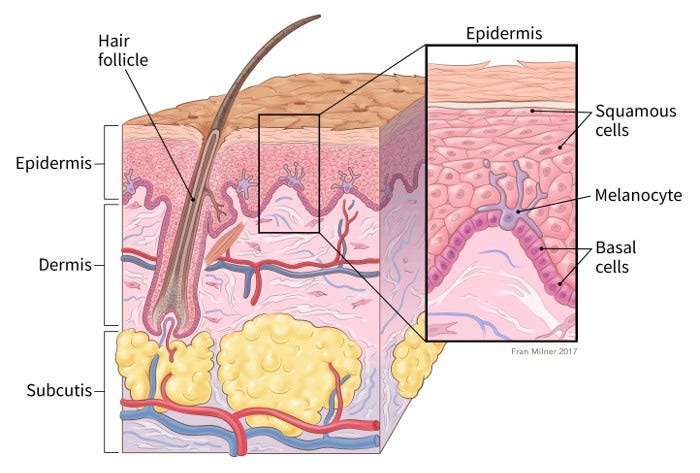
UVB rays are absorbed primarily by the top layer, the epidermis. UVB rays are associated with sunburn and are the major contributor to development of skin cancer. However, UVA rays, which penetrate into the dermis, can further exacerbate and contribute to skin damage, including cancers and aging.
UVB and UVA radiation can cause cumulative DNA damage and abnormal cell behavior.
I previously discussed that cancers are diseases of accumulated mutations, which can be inherited (genetic) or acquired through lifestyle factors. When mutations occur in important genes, this can cause cells to behave abnormally and grow uncontrolled. There are over 400 different identified genes linked to cancer progression. Not all are involved in every cancer, and some genes play a larger role than others.
Genes that are directly linked to cancer are those that are involved in correcting random errors in DNA or regulating cell growth and division:
DNA Repair Enzymes
Tumor Suppressor Genes
Oncogenes
If these genes develop mutations, it means they may not be able to regulate the important processes that prevent cancers from developing.
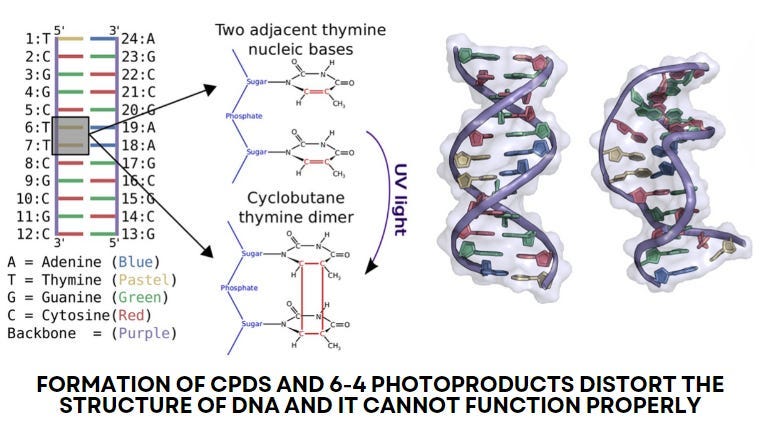
UVB radiation causes DNA damage directly.
When UVB rays penetrate the epidermis, the energy they contain causes specific damage to DNA: cyclobutane pyrimidine dimers (CPDs) and 6-4 photoproducts.
CPDs occur when adjacent pyrimidine nucleotides (either cytosine or thymine) in a segment of DNA detach from the double helix and bind to each other, forming a ring (cyclobutane).
6-4 photoproducts occur when adjacent pyrimidine nucleotides in a segment of DNA disconnect and bind between the 6th carbon of one and the 4th carbon of the other. This typically only occurs between thymine and cytosine or two cytosines.
Both errors cause distortion to DNA within the affected cell and interferes with structure and function of that DNA as a result.
UVA radiation causes indirect DNA damage through oxidative stress.
UVA rays penetrate deeper layers of the skin such as the dermis. UVA energy can be transferred to molecules in the skin such as flavins and porphyrins. Those molecules then transfer energy to oxygen (O₂) in skin cells, which converts molecular oxygen to reactive oxygen species (ROS).
ROS are highly reactive because of their structural instability. UVA can catalyze the production of singlet oxygen (¹O₂), superoxide anion (O₂⁻), hydrogen peroxide (H₂O₂), and hydroxyl radicals (OH•). These molecules react with DNA and cause structural changes in DNA by attaching these oxygen molecules to nucleotides.
8-Oxo-7,8-dihydroguanine (8-oxoG), is formed when (OH•) adds an oxygen to guanine, changing the structure and function of DNA. This can lead to the wrong nucleotide being added to a growing DNA strand during DNA replication.

We have cellular mechanisms to repair DNA damage.
Our body is pretty good at repairing cellular and molecular damage. We have a variety of mechanisms to monitor the our cells and initiate repair or self-destruction processes (if repairs aren’t possible). For UV-induced DNA damage, our cells typically use nucleotide excision repair (NER) and base excision repair (BER).
Very quickly: a trip around DNA. DNA is a double helix with specific sequences of molecules that dictate our genes. These molecules are called nucleotides, which are made up of a phosphate group, a deoxyribose sugar, and a nitrogenous base. There are (4) different nitrogenous bases in DNA: guanine, cytosine, adenine, and thymine.
Nucleotide excision repair (NER) cuts out the entire nucleotide molecule, whereas base excision repair (BER) only cuts out the incorrect nitrogenous base (G, C, A, or T). Enzymes proofread DNA and detect errors, which signal to additional enzymes to remove the incorrect regions and synthesize replacement DNA to fix the errors.
NER repairs bulky, helix-distorting DNA damage like cyclobutane pyrimidine dimers (CPDs) and 6-4 photoproducts which can be caused by UVB radiation.
BER repairs smaller DNA damage like 8oxoG as a result of oxidative damage caused by UVA radiation.
I won’t get into the really granular stuff here, but suffice to say that your body is pretty efficient at fixing errors in DNA. If it is unable to, your cells can also sense that and initiate programmed cell death: as we don’t want cells that are defective replicating in our bodies.
If DNA damage occurs in genes that help regulate cell repair and division, it can facilitate cancer development.
UVB and UVA radiation targets our cells pretty indiscriminately. It’s random which segments of DNA are potentially damaged by excess UVB and UVA exposure. That being said, genes that have higher proportions of adjacent pyrimidines might have higher likelihood of damage from UVB, whereas genes with high proportions of guanine nucleotides may experience higher impacts from UVA radiation.
Cancer doesn’t occur from one single insult to your cells or your body though. Cancer is a disease that progresses as a result of cumulative errors or mutations, specifically in genes that are related to controlling cell survival and growth.
For example, mutations in the tumor suppressor gene TP53 leads to defects in the p53 protein, which is critical to regulate programmed cell death of damaged cells. If it can’t do that, abnormal cells may grow uncontrolled, which can lead to cancer. Mutations in the BRAF gene impact the B-raf protein, which regulates cell division and survival. If B-raf no longer functions, those cells can grow uncontrolled as well.
Cancers most often occur as a result of multiple mutations.
A single excess exposure to UV radiation isn’t going to automatically cause cancer, and on the flip side, someone else could have years of excess UV exposure and never develop cancer. There are factors outside your control, but a large body of evidence shows that excess UV exposure increases the risk of all types of skin cancers.
Skin cancer is the most common cancer in the US, but there are different categories:
Carcinomas are cancers of epithelial cells and account for the vast majority of skin cancers.
Squamous cell carcinoma (SCC) are cancers of squamous epithelial cells (thin flat cells that form the skin surface) and account for about 15% of skin cancers.
Basal cell carcinoma (BCC) are cancers of basal epithelial cells (the lowest layer of the epidermis) and account for about 80% of skin cancers.
Melanomas are cancers of our melanocytes, specialized pigment cells in our skin and account for around 1% of skin cancers. However, melanomas cause 75-80% of skin cancer deaths.
It is estimated that between 80 and 90% of all skin cancers are caused by excess and long-term exposure to UV radiation.
(There are less common cancers like Merkel’s cell carcinoma and Kaposi sarcoma)
Many cases of skin cancers can be preventable
If you’ve gathered by now, a major modifiable risk factor for skin cancers is UV radiation from sun exposure. But we can take steps to reduce that exposure and the subsequent risks of skin cancer!
Sunscreens, especially those that provide UVA and UVB protection, reduce risk and rates of skin cancer.
Sunscreens, whether chemical (organic UV filters) or mineral (inorganic UV filters) protect us from the energy of UV radiation. They do this by containing active ingredients that are able to absorb UV energy and convert it into heat that is released. As such, the energy that would have penetrated your skin and potentially damaged DNA is transferred to the molecules in sunscreens.
Regular use of sunscreen has been demonstrated to reduce risk of skin cancers. Data suggest that daily use of sunscreens can reduce risk of SCC by 40% and risk of BCC by 15-30%. Similarly, regular use of sunscreens with 15 SPF or higher can reduce risk of invasive melanomas by 50%.
Other interventions that can further reduce risk are: wearing clothing with UV protection, seeking shade when UV index is higher, and wearing sunglasses, hats, and using umbrellas when appropriate (see more on Dr. Michelle Wong’s piece on risk mitigation).
We must also combat misinformation about skin cancer and sunscreens.
Chemophobia is a central theme in topics I discuss, so it’s no surprise it crops up when it comes to skin cancer. Everywhere you turn, people make unfounded claims about the risks of sunscreens, the harms of ingredients, and other pervasive misconceptions. While anti-science activist groups that target sunscreens intentionally, misinformation is further spread by medical professionals, including dermatologists. This authority gives falsehoods more legitimacy, allowing the fear-based myths to become more pervasive. More on this to come, but for now, please be assured that sunscreen, whichever type you choose, is a safe and effective method at reducing risk of skin cancer, and it is NOT causing cancer when you use it.
Thank you for supporting evidence-based science communication. With outbreaks of preventable diseases, refusal of evidence-based medical interventions, propagation of pseudoscience by prominent public “personalities”, it’s needed now more than ever.
Stay skeptical,
Andrea
“ImmunoLogic” is written by Dr. Andrea Love, PhD - immunologist and microbiologist. She works full-time in life sciences biotech and has had a lifelong passion for closing the science literacy gap and combating pseudoscience and health misinformation as far back as her childhood. This newsletter and her science communication on her social media pages are born from that passion. Follow on Instagram, Threads, Twitter, and Facebook, or support the newsletter by subscribing below: