Vitamin D: Can we Finally Stop Beating this Dead Horse?
Vitamin D deficiencies are vastly exaggerated and supplements don't improve health outcomes, but this belief has a very seedy underbelly
The wellness industry is a convergence of logical fallacies, lack of regulatory oversight, financial motives, and preying on the desire to do what’s best for our health. It brings in $5.6 Trillion every year and is wildly unregulated. Products range from relatively benign (vitamin supplements) to the seriously harmful (IV infusions, ozone enemas, urotherapy). Many utilize a common tactic in pseudoscience: make claims based on a grain of truth, and this will give you immediate credibility.
Vitamin D is a poster child of this. Yes, it’s an essential micronutrient. Yes, it is critical for key cellular processes. Yes, deficiencies can cause issues like rickets.
The hype around vitamin D supplementation and how common deficiencies are was a deliberate effort to profit off of misleading people.
This has become entrenched into clinical practices and popular culture. But the reality is, there isn’t evidence to support either statement…and after thousands of studies wasting trillions of research dollars, it is not for lack of trying.
Join me for a bit of a wild ride. Let’s start with the basics.
Vitamins are defined as carbon-containing (the scientific definition of organic) biologically important chemicals that we obtain through diet. While vitamin D is lumped into this category, we do not need to consume it. In fact, we can produce all the vitamin D we need, which happens to only be miniscule amounts.
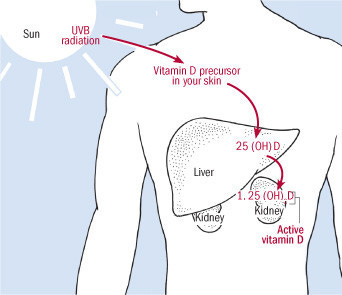
Vitamin D is a fat-soluble vitamin that we produce through sun exposure, specifically, UVB radiation. The multi-step process starts when 7-dehydrocholesterol is converted into previtamin D3 after absorption of UVB radiation in our skin. Previtamin D3 rapidly changes into vitamin D3 (cholecalciferol), and is enzymatically converted into hydroxyvitamin D (25(OH)D) in the liver. This is the form of vitamin D that is measured in blood tests, but is not the bioactive form. 25(OH)D is further converted into the active form 1,25 dihydroxy vitamin D (1,25(OH)2D, or calcitriol) in the kidneys.
Vitamin D participates in numerous physiological processes.
Bone health. Aids in calcium absorption, helps regulate calcium and phosphate levels in the blood for bone mineralization and muscle function, aids in bone growth and remodeling, and protects against disorders of bone such as rickets, osteomalacia, and osteoporosis.
Immune system function. Aids in regulation and function of immune cells, modulates cellular growth and division, mediates inflammatory signaling.
Glucose metabolism. Aids in insulin secretion from the pancreas.
…and more.
Just minutes of sun exposure enables us to make the vitamin D we need. You’d only need 3 to 8 minutes of outdoor exposure with 25% of your skin exposed in Boston from April to October to synthesize sufficient supply. But the other cool thing is that…
We maintain stores of vitamin D in our liver and fat cells, where it can be utilized if needed.
This ensures adequate vitamin D even when sun exposure is limited. We have multiple conduits for vitamin D. The first and evolutionarily preferred: synthesize from UVB exposure. Next: surplus is liberated from liver and fat cells. Finally, dietary sources: fatty fishes like salmon, mackerel, sardines, egg yolks, red meat, and liver, and fortified dairy products and cereal grains. These ensure that pretty much everyone has sufficient vitamin D.
Vitamin D deficiency is not nearly as prevalent as many believe
Every time I discuss dietary supplements, the comments roll in:
“But I live up north, and it is dark most of the winter. My doctor told me to take a vitamin D supplement.”
“I work indoors and in the winter, I almost never see the light of day. How can you say I am not deficient?!
These comments underscore bigger issues at play.
Healthcare providers are human, and are prone to getting stuck in habits, even if they aren’t supported by evidence. While we want healthcare providers to utilize the best quality science, we know that isn’t always the case. As a result, they, and members of the general public, fall into common refrain about the ubiquity of vitamin D deficiency.
Some of this isn’t your fault, or your doctor’s fault, because there’s been an active misinformation campaign about vitamin D.
What actually qualifies as vitamin D deficiency?
The Institute of Medicine (IOM) reviewed data relevant to vitamin D levels, health outcomes, supplementation benefits, to set specific levels to define vitamin D deficiency. This was published in an 1,100 page report in 2010 (find the full report to download here).
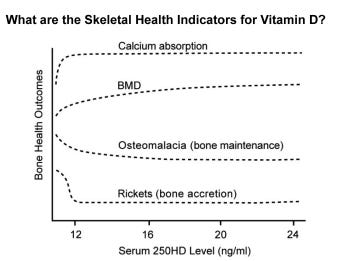
IOM set a conservative threshold of 20 ng/mL (50 nmol/L) circulating vitamin D. Their analysis of the data suggest 12 ng/mL is more than sufficient, but levels ensure inclusion of outlier populations. Even when evaluating clinical skeletal health outcomes, there is a plateau at 12 ng/mL 25(OH)D, and outcomes do not improve above 20 ng/mL. IOM also found no evidence of benefits of serum vitamin D levels above 20 ng/mL (remember, these are 25(OH)D levels, as measured by blood test. This doesn’t include reserves in liver and fat cells).
Population data from 2001-2018 demonstrate that 97.5% of Americans have 25(OH)D levels above 25 ng/ml, a cutoff higher than the IOM benchmark.
What about people with darker skin? A cursory glance at raw data suggest 25(OH)D levels are lower in Black Americans, but these populations generally have no clinical symptoms of vitamin D deficiency.
Blood tests assess 25(OH)D bound to vitamin D-binding protein, which typically accounts for about 85-90% of 25(OH)D in circulation. The non-bound 25(OH)D, called bioavailable 25(OH)D, is a smaller fraction. People of African ancestry have higher proportions of gene variants that facilitate more of bioavailable 25(OH)D, and standard tests underestimate total vitamin D levels. When considering all forms of 25(OH)D, the levels of vitamin D were similar among groups. So in reality, while Black people are commonly assumed to be vitamin D deficient, this is unlikely to be true.
So if nearly 20 years of data demonstrate that the vast majority of people aren’t at risk, why do so many people, even healthcare providers, continue to repeat the refrain that vitamin D deficiency is widespread?
The Endocrine Society (and laboratory tests) inflated the threshold for deficient vitamin D levels
This is where the story gets really juicy, so buckle up.
After IOM published their 1,132 page analysis in 2010 and defined baseline for clinical vitamin D deficiency - levels that cause medical issues directly linked to vitamin D - a guy decided he had to undermine it - and there was a motive behind his actions.
In 2011, a physician named Michael Holick published a paper in the Journal of Clinical Endocrinology & Metabolism as a figurehead for the Endocrine Society.
He claimed vitamin D deficiency is a widespread '“pandemic”, the threshold set by IOM was too low, and people needed to get routine testing and take supplements to address deficiencies. He used a single observational study, which looked at 675 adult males, and noted that about 25% of them had osteomalacia. The study didn't detect bone problems in people with 25(OH)D levels 30 ng/ml: therefore, that was the threshold Holick stated should exist.
Association does not equal causation
Holick cherry-picked a small and comparatively weak study while ignoring more robust data and this had far-reaching consequences. While his claims were unsupported, the Endocrine Society adopted his position, as did physicians, hospitals, Quest Diagnostics, LabCorp, and other commercial labs. Commercial labs raised their testing threshold to 30 ng/mL, 1.5-fold higher than the level set by IOM, artificially flagging people as ‘deficient’ who are not.
The inflation of testing thresholds caused surges in vitamin D testing and purchase of vitamin D supplements after ‘low vitamin D’ results. The US Preventive Task Services has stated that there is a lack of evidence for benefits of vitamin D testing in adults with no symptoms of deficiency.
Higher vitamin D levels are not equated with improved health, and people are being misled. More than that, they are operating with undue health anxiety and spending needless money on things that are not supported by data.
Michael Holick has a motive behind promoting vitamin D
Holick’s 2011 paper trying to shred IOM was not his only - he has since written other papers citing his work to flood the field.
But before the IOM report, he wrote a book called “The Vitamin D Solution” where he promoted excessive supplementation, routine blood tests (he listed out-of-pocket prices for convenience to his readers, how generous), and foments fear about vitamin D deficiency and all the medical issues that will occur as a result: cancer, autoimmunity, chronic disease, bone disease, etc.
It would have been hugely detrimental to his book sales if the IOM report and recommendations were implemented widespread. As such, it was necessary to attack it and use his influence with the Endocrine Society to undermine it.
Holick has made millions of dollars propagating false claims, from book sales, ‘consultation fees’ from supplement companies, commercial labs, speaking engagements, and more. He even received money from tanning bed organizations.
If you do not have clinical symptoms of a vitamin D deficiency, why would you believe you are deficient?
The Vitamin D ‘industry’ is a huge moneymaker
Michael Holick’s unsubstantiated claims have been legitimized by many in healthcare and promoted by wellness warriors like Mehmet Oz, Gwyneth Paltrow, GOOP, Oprah Winfrey, and others. Profits have skyrocketed. Vitamin D supplement sales in the US were $1.49 Billion in 2020, up from $936 million in 2017, and forecasted to continue to grow by 7.34% year over year, a 10-fold increase in just a decade.
Vitamin D testing has similarly exploded. Over 10 million vitamin D tests were ordered for Medicare patients in 2015, up 547 percent since 2007, costing $337 million. It is the fifth-most ordered lab test but between 25% and 77% of them, even among older adults, have no clinical indication. Direct-to-consumer tests also use the false benchmark of 30 ng/ml. Some inflate it more. InsideTracker uses a range of 30-75 ng/ml, and falsely claims IOM set that threshold. Athlete Blood Test states that they ‘decided’ to ignore scientific experts and set their level at 50 ng/ml, just for funsies. The direct-to-consumer vitamin D testing market was $848 Million last year, and each test can run from $15 to $499.
It is hugely lucrative to continue to propagate the fallacy that vitamin D deficiency is widespread.
There is some good news: medical organizations, including the Endocrine Society, are finally catching on.
Numerous professional organizations, including USPTF (noted previously), the National Academy of Medicine, the American Board of Internal Medicine (ABIM) Foundation, and the American Society for Clinical Pathology (ASCP) all now endorse a position of
“Do not order population-based screening for vitamin D”
to more appropriately reflect the fact that these tests are medically unnecessary, waste money, time and resources, and contribute to the false belief of widespread vitamin D deficiency.
In addition, the Endocrine Society is completely revising their guidance on vitamin D, tossing out Michael Holick’s cherry-picked profit-driven claims, and using only robust randomized controlled and clinically relevant data. A win for science!
It is actually a bit sad, because in his early career, Holick was on the leading edge of research related to vitamin D, but has since promoted extreme beliefs that have harmed collective health. Unfortunately, this is more common than people realize.
Vitamin D deficiency is overstated, tests inflate the proportion of people who believe to be vitamin D deficient, but we also know that vitamin D is critical for cellular processes. If people operate under this assumption (even if misguided) and decide to take a supplement, does it help?
Vitamin D supplementation does not improve health outcomes
Sorry to be the bearer of bad news, but there have been countless high-quality randomized controlled trials evaluating potential causative links between vitamin D supplementation and health outcomes. You can always find a weaker or poorly designed study to support something, but that is why the quality of evidence matters. Based on the body of data: vitamin D supplementation does not benefit health.
It doesn’t prevent infectious respiratory illnesses, reduce symptom severity, including for COVID-19.
It doesn’t help prevent cardiovascular disease, atrial fibrillation, or other heart conditions.
It doesn’t prevent cancers, including colorectal, primary invasive, and in situ carcinomas.
It doesn’t prevent falls, bone fractures, or improve bone mineral density.
It doesn’t reduce the risk of developing type 2 diabetes.
It doesn’t moderate body composition or reduce knee pain.
It doesn’t improve age-related macular degeneration, cognitive function, or headache frequency.
It doesn’t improve athletic performance.
It doesn’t even reduce all-cause mortality rates.
See more RCTs and meta-analyses here.
There are exceptions. For newborns at least partially breastfed vitamin D supplementation is beneficial. Those with certain digestive or excretory diseases that impact absorption or storage of vitamin D may benefit (e.g. Crohn's disease, cystic fibrosis, celiac disease, and certain liver and kidney diseases, those who had gastric bypass surgery).
On the flip side, there are risks associated with excess vitamin D.
Everything has a safe dosage and everything has a harmful dosage.
There is such thing as too much of a good thing. Even vitamin D can be toxic at a certain dose. Risks of excessive vitamin D include:
Hypercalcemia (high calcium levels) leading to nausea, vomiting, muscle weakness, psychiatric issues, inappetence, dehydration, excessive urine production (polyuria), excess thirst, and kidney stones.
Increased risk of dangerous falls (muscle and neuronal function impairment)
Levels as low as 50 ng/ml may be associated with increased risk of death and incidence of certain cancers.
Vitamin D toxicity can cause renal failure, calcification of soft tissues in the body (including coronary vessels and heart valves), cardiac arrhythmias, and death.
Vitamin D toxicity occurs from supplement overdose (sometimes due to false labeling of the product, another issue with lack of regulatory oversight), excessive self-dosing due to misinformation, or incorrect recommendations from healthcare providers. Excess sun exposure is not a contributor, because we have evolutionary and regulatory ways to keep that in check.
I get it. It is hard to let go of strongly held beliefs, especially when they are echoed by so many in our society. The good news: scientific and medical experts are starting to shift after the profound attention and financial investment into vitamin D have no supported these beliefs.
While for most people, taking a supplement is low risk, the reality is, there’s no reason to expend your time, energy, and money on something that isn’t improving your life. That’s the goal after all, isn’t it?
I hope this somewhat long deep dive was useful for so many who have had questions about vitamin D specifically. This is a free and public article, so please feel free to share it with your friends and family!




I often think about how the rising costs of healthcare also contribute to this problem. I think people get desperate for alternatives when they can’t afford medical care. Not necessarily a global issue, but definitely an element of truth to it in the USA.
Really interesting article. Are there conditions where more vit D is needed? Because over the last years i really felt like shit and were sick every two weeky in phases where i took no or less vitamin D. Somehow even with 5000 IUs per i experienced this. Somehow with 7000 to 10000 IUs per Day i feel great. I know its anectotal and science says different, but thats how it was and is for me. With the level of 13ng/ml i had 7 sinusitis in a row. Since im taking high vit D (now 80ng/ml) i had zero. So don't know what to do. If im taking it away and lowering i will feel bad agin. Maybe you have an idea what i can do? (since. Most physicians also have no clue)
Greetings