Lyme Disease: fraudulent tests are rampant
Lyme disease is frequently over-diagnosed or misdiagnosed as a result of inaccurate and unproven consumer tests.
While Lyme disease is a public health concern, rampant misinformation has led many in the general population to perceive it as a much bigger threat than it is.
Some of you may know that I started doing Lyme disease research, as far back as my undergraduate days at Stony Brook University, nearly 20 years ago. I investigated the immunology of infection for my PhD dissertation research, where I was immersed in the fascinating science, but also the pseudoscience, that plagues the field.
It is ultimately why I agreed to become the current Executive Director of the American Lyme Disease Foundation: to help combat misinformation around Lyme.
Lyme disease is an acute bacterial infection caused by Borrelia burgdorferi (rarely Borrelia mayonii) in the United States and Borrelia garinii and Borreli afzelii in Europe, which are transmitted through the bite of infected ticks.
Yes, it is the most common vector-borne disease in the United States, but let’s look at the numbers. There are about 30,000–50,000 confirmed cases of Lyme disease reported in the United States every year. The Centers for Disease Control and Prevention (CDC) generously estimates that up to 475,000 people could be infected annually.
(That “could” is an important word here: that estimate is based on people actively seeking treatment and antibiotic prescriptions for Lyme, behavior that is heavily influenced by public perception and misinformation found online.)
But let’s use 475,000 for the sake of discussion. That is 0.14 percent of the U.S. population. So yes, while it is more common than other tick-borne diseases such as Rocky Mountain Spotted Fever, Anaplasmosis, or Powassan virus, Lyme is still not that common. Compare this to the 45 million Americans who get the flu every year—a 100-fold higher case rate—to put things into perspective.
Unfortunately, Lyme disease is frequently over-diagnosed or misdiagnosed among individuals who do not currently or actually have Lyme disease, and as a result, antibiotic prescriptions are also issued when unnecessary. In many instances, it is even self-diagnosed, as a result of actively seeking out information to support one’s confirmation bias.
In order to correctly diagnose Lyme disease, multiple factors must be considered.
When diagnosing someone with Lyme disease, or even considering a potential diagnosis of Lyme disease, an appropriate differential needs to be considered.
First and foremost, clinicians must consider the symptoms the patient presents with and how they align with those of Lyme disease.
Lyme disease mostly presents with generic symptoms that are observed in many other infections and non-infectious ailments, including fever, headache, muscle aches, fatigue, chills, joint pain, and swollen lymph nodes. The Erythema migrans (EM) rash, which radiates from the site of the tick bite, is the only true clinical differentiator, and this presents in 60-80% of cases (although some people may not notice it). There are also other conditions that can cause EM, so those must be factored in as well.
If a person has one of more of these symptoms, clinicians must consider the likelihood that the patient has been bitten by a tick carrying Borrelia burgdorferi, the bacterium that causes Lyme disease.
This must be weighed by the geographic region they were in. There are places that Lyme disease simply does not exist. In order for someone to get infected with B. burgdorferi, not only do the right species of ticks need to be present, but the bacteria need to be found in those ticks.
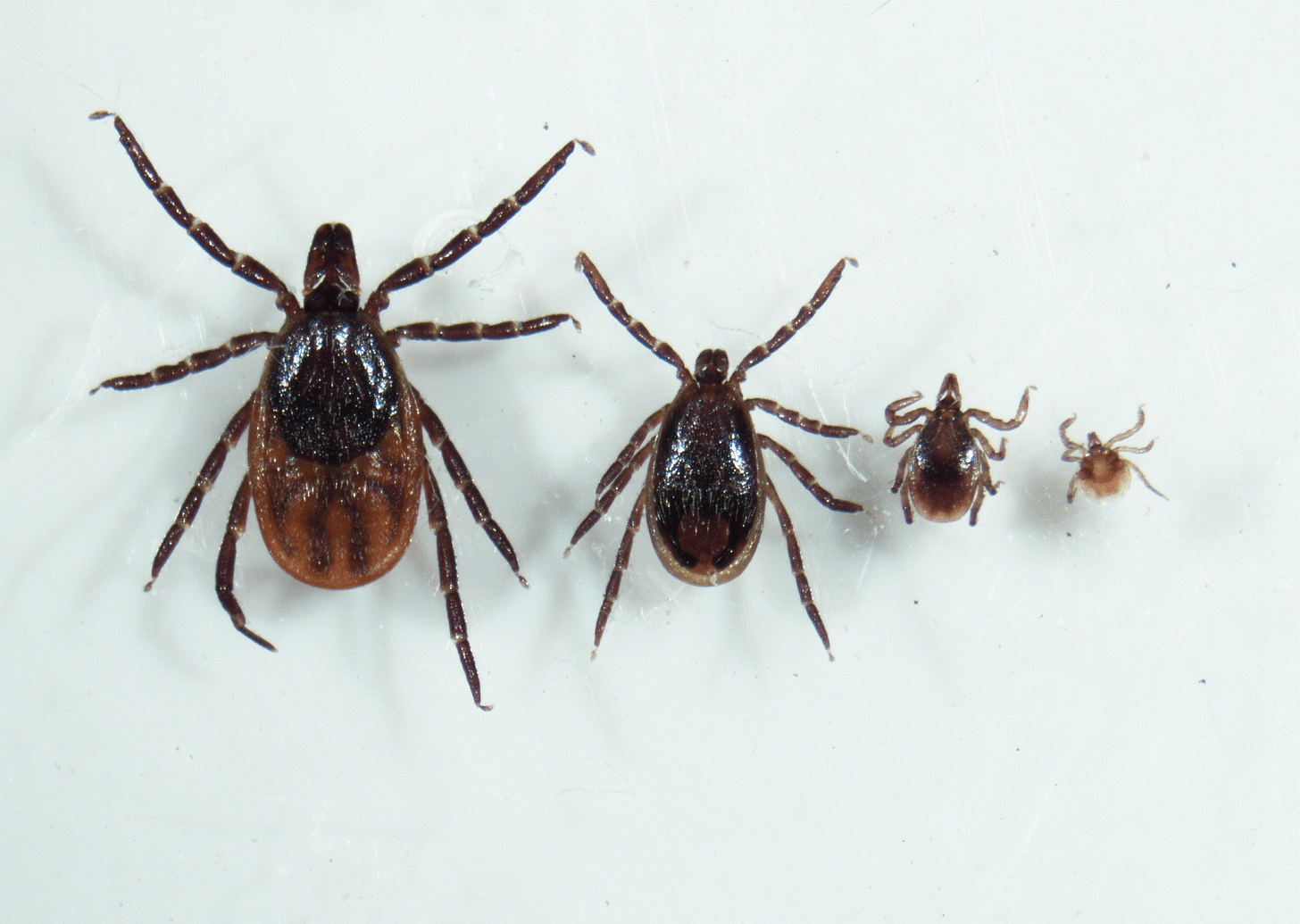
There are only 2 species of ticks in the US that are able to transmit B. burgdorferi to humans, the black-legged tick (Ixodes scapularis) and the Pacific black-legged tick (Ixodes pacificus). These do not live everywhere in the US, and Lyme disease does not exist in parts of the world outside North America and Europe (in Europe, Lyme disease is caused by Borrelia garinii and Borrelia afzelii). So if a person from Australia is claiming they have Lyme disease, the true likelihood of that is EXTREMELY low, especially if they have no recent travel to places where Lyme disease even exists. Lyme disease is not transmitted person-to-person either, and is not transmitted by other arthropods (like mosquitoes), or through sexual contact (all rumors I’ve heard through my years of doing Lyme research).
Next, clinicians will consider other illnesses that may cause similar symptoms and the likelihood that the symptoms are a result of one of those.
Since the symptoms of Lyme disease are very generic, there are a lot of things that can also cause similar symptoms: mild viral infections, autoimmune disorders like multiple sclerosis and rheumatoid arthritis, other infectious diseases that are unrelated, and even psychiatric disorders. Lyme is very frequently used as a scapegoat to explain generic symptoms, even if a person had no epidemiological factors that would indicate a possible B. burgdorferi infection. Not only does this propagate misinformation about the prevalence of Lyme disease, it can also mean that people are not getting treatment for other medical issues.
Finally, if the likelihood that the individual may have LD is high, laboratory testing is ordered.
It is important to recognize that these tests do not detect active infection or the bacteria, but rather, an indication of an immune response against the bacteria. The tests are assessing the presence of antibodies that your immune system produced after encountering the bacteria from venous blood samples. This means that they cannot tell if an individual is currently infected or had been infected in the past.
Just like COVID-19 antibody tests, a positive result can mean you could have had a recent infection, or one well in the past.
You should not be tested for Lyme disease if you only have muscle pains, do not exhibit other symptoms, and have no history of B. burgdorferi exposure.
The FDA-approved Lyme disease diagnostic test is a two-step protocol. This consists of an initial enzyme-linked immunosorbent assay (ELISA) followed by a specific Western blot assay. Both are detecting the presence of antibodies in blood samples and can allow determination of a recent (current) or past infection.
In step 1, a test called enzyme-linked immunoassay (ELISA) is used, which is less specific than the Western blot used in step 2.
If an individual tests negative on the initial ELISA, it is unlikely they have Lyme disease now or in the past.
If an individual tests positive on ELISA or the results are indeterminate, they move to step two of testing. Step 2 uses a Western Blot looking for specific types of antibodies against Borrelia burgdorferi. The Western blot detects two different classes of antibodies, IgM (earlier antibodies after infection), and IgG (later antibodies after infection). A positive result indicates the individual has Lyme disease (or had in the past), whereas a negative result indicates that step one was a false positive.
A Western blot assay that detects both IgM and IgG should be performed if the individual is being evaluated within 4 weeks of symptom onset. If it is beyond 4 weeks of symptom onset, only the IgG can be performed, since IgM antibodies decline rapidly during the immune response to infection.
Interpretation of the Western blot assay is based on the number of bands detected for each of the antibody isotypes (different structural variants of antibodies produced during an immune response). The IgM Western blot result is considered positive if 2 of the 3 bands tested are present. In the case of the IgG Western blot, the result is designated as positive if 5 of the 10 bands tested for are present.
As of 2019, CDC and FDA have cleared select two-tiered options that utilize ELISA in both steps, but again, similar criteria are applied. Sometimes, these tests yield false positive results in step 1, and indeterminate results in step 2. The bacteria are complex, and the immune response they elicit is also complex, so diagnostics have always been a challenge. As mentioned, it’s not like strep throat where there’s tons of bacteria and you can swab and culture them easily.
This complexity has opened the door for a lucrative market of inaccurate and unapproved tests claiming to diagnose Lyme disease.
Fraudulent Lyme tests, are often called “non-standard” Lyme tests, are sold by private commercial labs, and are not FDA-approved or accurate in any way. You should avoid labs claiming to do “Non-Standard” LD testing.
Testing using urine or other non-blood bodily fluids are not accurate and are not FDA approved. They are often sold direct-to-consumer (including at common pharmacies). They frequently claim to diagnose Lyme disease alongside an array of other infections, many of which are implausible co-infections such as Bartonella, Ehrlichia, and more.
Many of these fraudulent tests that are sent out to fake diagnostic labs almost always return a “positive result” for the individual being tested, resulting in many people being diagnosed with Lyme disease who did not and do not have Lyme disease.
These tests are often ordered by self-proclaimed Lyme specialists (sometimes “Lyme literate MDs”) who are the opposite of Lyme literate. Many are not credentialed clinicians, but chiropractors, naturopaths, or similar. Even those who have medical degrees are often not infectious disease specialists.
They profit off these tests that are not covered by insurance (because they lack evidence to support them), which they promote when people have no reason to suspect Lyme. The lucrative market of fake tests causes people to undergo unproven and expensive treatments outside standard antibiotics that are ineffective and potentially harmful.
It is critical to understand that testing for Lyme disease using urine or other non-blood bodily fluids are not accurate and are not FDA-approved. There are no data to support their use, and they have not been validated for accuracy at all.
There are no approved direct-to-consumer tests for Lyme disease, so any tests you find at CVS, Walgreen, etc., are not valid tests to use. In order to get an accurate diagnostic test, you must go through a clinician that uses an FDA-approved diagnostic Lyme disease test.
Labs that promote non-standard and unapproved Lyme tests are widespread
Unfortunately, it can be very difficult for the public to discern what’s credible and what’s not. When it comes to commercial labs selling fake Lyme disease tests, that is all too often that. That is why several of them have had lawsuits brought against them.
IgeneX is a key one that has been particularly criminal. Practitioners that promote the false notion of a chronic infection sent patient blood samples to this California lab, which was once investigated by Medicare and the state of California for pumping out too many positive tests. In 2001 the federal Office of the Inspector General put Igenex on a list of noncompliant labs. While it paid some fines, the lab is still functioning and performing the same things to this day.
While some of these labs may provide legitimate medical diagnostic services for other tests, they all offer and sell non-standard and unvalidated tests for Lyme and other pseudoscience diagnoses. These include:
DNA Connexions
Galaxy Diagnostics
Medical Diagnostic Laboratories (MDL)
Milford Molecular Diagnostics Laboratory
Global Lyme Diagnostics
Pharmasan Labs (iSpot Lyme)
Coppe Laboratories (myLymeTest)
Moleculera Labs (Cunningham Panel)
Lyme Diagnostics Ltd.
Vibrant America/Vibrant Wellness
and any other lab on Quackwatch’s list of “Laboratories Doing Nonstandard Laboratory Tests“.
Lyme disease is an acute bacterial infection that is treatable with antibiotics
After a course of antibiotics, any bacteria that existed during infection are killed, and the infection is eliminated. In fact, clinical studies evaluating the efficacy of longer term antibiotics have failed to find a benefit. There is no evidence that in humans, B. burgdorferi exist as ‘latent’, ‘persisters’, or biofilms in the body.
While a small proportion of individuals report symptoms that last after finishing treatment, this has long been characterized as post-infection sequelae: something that is not unique to Lyme either.
Unfortunately, this has been used to spread misinformation about Lyme disease, and, as a result, has led to a huge market of fraudulent tests that mislead people about what may truly be causing their symptoms. Aside from the fact that these are expensive and not covered by insurance, Lyme pseudoscience causes harm to individuals based on false information. It erodes public health and trust in science, and it can lead people to delay care for medical conditions that are falsely attributed to Lyme. We have a duty to combat this type of predatory pseudoscience, even if it has a loud voice.
Read more at the American Lyme Disease Foundation website.
Thanks for joining in the fight for science!
Thank you for supporting evidence-based science communication. With outbreaks of preventable diseases, refusal of evidence-based medical interventions, propagation of pseudoscience by prominent public “personalities”, it’s needed now more than ever.
Your local immunologist,
Andrea







Your article went in the opposite direction from what I expected. I was thought to have arthritis, over 50, in inflamed knees. I went to an orthopedic doc. and after a second look at X-rays thought to have me tested for Lyme. It came back positive. I live in SW Pa. I never heard of fake testing.
Thank you for this content! Reading your blog and listening to the Lyme podcast with Unbiased Science I have a question about what happens when Lyme isn't treated with a course of antibiotics in a timely manner? This is where I could see the notion of "chronic Lyme" come into play and wonder what actually does happen when Lyme isn't treated?