Guess what? We can prevent some cancers through vaccination.
Are you concerned about media headlines regarding "rising rates of cancer" but haven't gotten an HPV vaccine?
Media headlines lately are all chattering about “rise” of cancer in young adults. Of course, many people are understandably concerned: the term cancer connotes fear. Of course, as the media is wont to do, they lump all cancers into a single bucket, and fail to note that many cancer rates are declining. If you want a quick overview of the diversity of cancers, read this piece.
One example? Rates of cervical cancers are plummeting, due solely to the HPV vaccine.
HPV, or human papillomavirus(es), cause 99% of cervical cancers. HPVs ALSO cause many causes of other cancers: anal cancers, penile cancers, oropharyngeal cancers, vulvar cancers, and vaginal cancers. And guess what? We have an incredibly effective vaccine that protects against these viruses, which subsequently PREVENTS CANCER.
Let’s talk about this more, instead of fear-mongering and clickbait.
Human Papillomaviruses (HPV) are a broad group of over 100 viruses that can infect different parts of the body.
HPVs are so named because papilloma means “small wart-like growth on the skin or mucous membrane”, and yes, some HPV strains lead to warts. Not just genital warts, either. Have you ever had a plantar wart on your foot? That’s caused by HPV.
HPVs are DNA viruses in the Papillomaviridae family. Because HPVs have DNA as their genomic material, they invade host cells and replicate their genome within the host cell nucleus (because that is where DNA resides and where the required machinery is located).
A unique feature of HPVs in contrast to other DNA viruses like Herpesviruses, is that HPV replicates its genome upon initial infection as an episome, or a separate piece of DNA from our chromosomal DNA. Remember this, because it’ll be important as we get further into the discussion.
Around 30 HPV types can affect the genitals, and 14 types are considered high risk for cancers, including cancers of the cervix, anus, penis, vagina, vulva and back of the throat (oropharyngeal).
Contrary to misconceptions, HPV affects both men and women & it is the most common sexually transmitted infection (STI) in the USA and in the world.
HPV is transmitted via skin-to-skin contact, which can be through sexual activities or other close contact. These activities can include genital, anal, and oral sex. It is not solely transmitted through penetrative sexual activity, mere direct physical contact is sufficient to spread virus to others.
Almost every unvaccinated person who is sexually active will get HPV at some time in their life. About 13 million Americans, including teens, become infected with HPV each year. More than 43% of American adults ages 18-59 are infected with genital HPV, and there are higher infection rates among men (45%) than women (40%).
As there are so many different HPV types, we often further stratify them into “non-oncogenic” (wart causing) or “oncogenic” (cancer-causing).
An oncovirus or oncogenic virus is a virus that can cause cancer.
In the case of HPVs, there are 14 high risk HPVs that can cause numerous cancer types. These include:
HPV 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, and 68.
HPV16 and HPV18 are responsible for most HPV-related cancers.
More than 99% of cervical cancer cases are due to HPV
Oncoviruses lead to cumulative mutations in our cells that ultimately cause dysfunction and dysregulation that allow cancer to progress. If you recall from my recent post on cancer basics, cancers of all types occur when our cells no longer behave as they should. In the case of HPVs, the viruses directly interact with our cell machinery which allows this to occur.
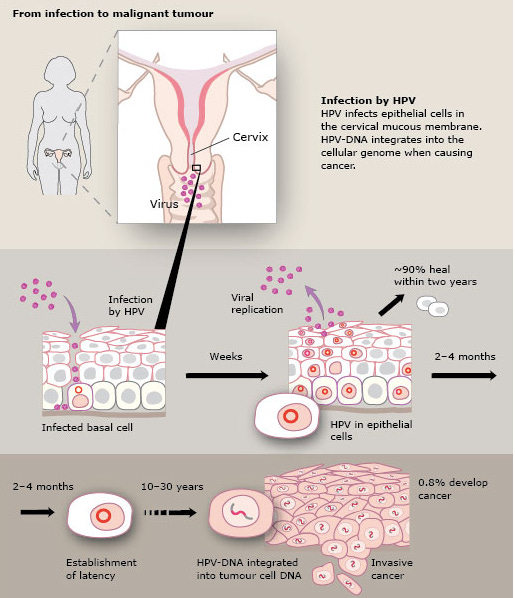
The progression from HPV to cancer takes time.
Broadly speaking, the progression from HPV infection to cervical cancer (and other cancers) takes 15-20 years in people with normal immune systems. For those with weakened immune systems, such as those who are transplant recipients or have untreated HIV infection, cancer can progress within 5-10 years.
HPVs that can lead to cancer are able to do so because the virus persists after infection, and is not cleared by our immune system. The high-risk HPV stays in your body and it has the ability to turn normal cells into abnormal cells (precancers) and then cancer.
Remember, cancers are diseases of cumulative mutations, where cells in our body no longer listen to cues they should. This process is not immediate, so you could be infected with HPV decades before you would develop the cancer caused by the virus.
HPV has cancer-causing proteins that interfere with normal cell function.
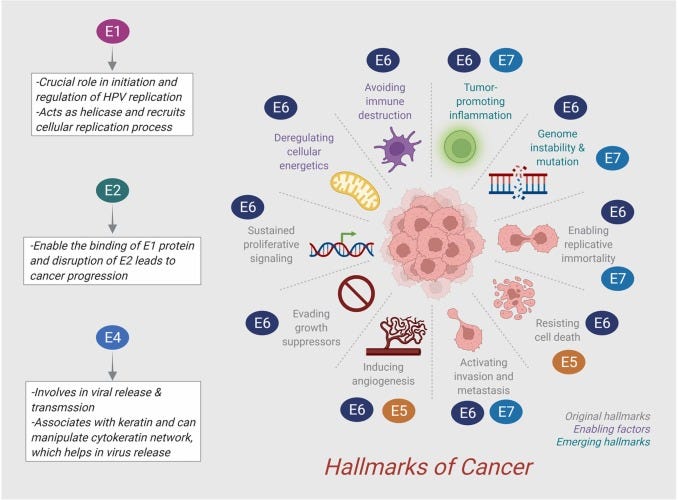
There are proteins produced by HPV that are important for cancer progression. These are referred to as oncoproteins (cancer-causing proteins). The key oncoproteins of HPV are called E6 and E7. E6 and E7 take charge of cellular checkpoints to establish cancer hallmarks such as uncontrolled cellular proliferation, angiogenesis (formation of new blood vessels), invasion, metastasis, evasion of apoptosis (that programmed cell death I spoke about), and inhibition of tumor suppressor genes. In the case of HPV, the primary action is on these critical tumor suppressor genes.
But once these proteins disable the tumor suppressor genes, the normal checks and balances that should occur in our cells no longer occurs. That means that mutations that occur as a result of errors in replication can persist, leading to more aberrant behavior in cells and the potential progression to cancer.
E6 protein promotes the degradation of the tumor suppressor protein p53.
When E6 interacts with and promotes the degradation of the tumor suppressor protein p53, this prevents p53 from being able to control and regulate the halt of cell cycle, replication, and programmed cell death when our cells experience mutations (DNA damage). By allowing cells with damaged DNA to continue dividing, this contributes to accumulation of mutations and the development of cancer.
E6 also binds to other cellular proteins involved in cell signaling and apoptosis, disrupting their normal functions and promoting cell survival and proliferation.
E6 also interferes with the function of cellular proteins involved in maintaining genomic stability and regulating cell growth such as DNA repair enzymes, another class of genes that are critical in the progression of cancer.
E7 protein promotes the degradation of the tumor suppressor protein retinoblastoma (pRb).
When E7 binds to the retinoblastoma (Rb) tumor suppressor protein, this promotes the degradation of this important protein, which is critical to regulate normal cell cycle of our cells. As a result, this can lead to uncontrolled cell proliferation even as DNA damage and cumulative mutations occur.
E7 impedes the function of other cellular proteins involved in cell cycle regulation and DNA repair, promoting genomic instability, accumulation of DNA mutations, and oncogenesis.
E7 also modulates the activity of transcription factors (proteins that regulate the expression of genes) and other cellular proteins involved in cell growth and differentiation.
In addition to E6 and E7, other HPV proteins are also indirectly involved in cancer development.
E1 and E2 are HPV proteins that regulate the replication of viral genome and protein transcription. As a result, E1 and E2 also promote the production of oncoproteins E6 and E7. E5 can also help induce angiogenesis, or the development of new blood vessels, which can feed cancer cells as a tumor is progressing. In addition, E5 facilitates survival of mutated and damaged cells, as opposed to inducing programmed cell death (which would occur in normal cells).
When these proteins act and interact with our cells, they override our normal cellular processes, leading to unregulated cell growth, mutations, and cancer progression.
HPV hijacks basal epithelial cells to cause cervical cancer.
Let’s discuss this process in the context of cervical cancer (while also remembering that HPV can cause other cancer types as well).
HPV primarily infects epithelial cells, which are found in the skin and mucous membranes in the genital tract, oral cavity, and respiratory tract. Within the genital tract, the basal epithelial cells of the squamous epithelium are the initial targets of HPV infection in the cervical mucosa.
HPV, just like all viruses, requires that viral capsid:host cell receptor interaction. In the case of HPV, the capsid proteins L1 and L2 bind to proteins on the host cell such as heparan sulfate proteoglycans (HSPGs) and integrin proteins.
Initially, HPV DNA replicates within the nucleus of those epithelial cells as an episome. However, if our immune system doesn’t clear the HPV infection, the HPV genome can establish latency and integrate its own DNA in the DNA in our cells. HPV utilizes several enzymes and other proteins to facilitate this.
As these infected basal epithelial cell divides, the viral genome is also are replicated and distributed into the daughter cells, which facilitates the continued spread of HPV, and the subsequent alteration in cellular processes as a result of those oncoproteins.
HPV typically infects differentiated epithelial cells in the ‘bottom’, or basal layer. However, as HPV leads to structural and functional changes in those cells, the cells move toward the surface of the epithelium, which can facilitate continued spread of HPV, cancer growth, and spread to other body sites.
The continuous attack by HPV causes pathological changes in cervical cells, leading to abnormal structure and function. These abnormal cells are called Cervical Intraepithelial Neoplasia (CIN), a precursor to cervical cancer. CIN is a term used to describe abnormalities in the epithelial cells of the cervix that have not officially become ‘cancer’. CIN is scored as 1, 2, or 3, depending on the extent of the changes in cells, and these are detected through Pap testing or HPV tests. The progression from CIN to cervical cancer typically occurs over a period of years to decades and involves several stages:
CIN 1 (mild dysplasia): CIN 1 represents mild abnormalities. The dysplastic cells appear abnormal, but are still confined within the basal layer of the epithelial membrane.
CIN 2 (moderate dysplasia): In CIN 2, the abnormal changes involve a larger portion of the epithelial layer and are typically extending into the lower two-thirds of the tissue.
CIN 3 (severe dysplasia or carcinoma in situ): CIN 3 is more advanced dysplasia, where the abnormal changes involve nearly the entire thickness of the epithelium. At this stage, the cells may appear highly abnormal and have the potential to progress to invasive cancer if left untreated. Carcinoma in situ refers to “cancer in place”, meaning that these are cancerous cells, but have not yet spread.
Invasive cervical cancer: If the abnormal cells progress beyond the epithelial layer and invade deeper into the cervical tissue or spread to other parts of the body, it is considered invasive cervical cancer. This is the most advanced stage of cervical neoplasia and requires prompt medical intervention.
The progression from CIN to cervical cancer is influenced by many factors, including the presence of high-risk human papillomavirus (HPV) infection, immune status, genetic factors, and environmental and lifestyle factors that further increase cancer risk.
Regular cervical screening is critical to detect and manage CIN at an early stage before it progresses to cervical cancer. Depending on the severity of the CIN lesions, treatment options may include surveillance, excisional procedures (such as loop electrosurgical excision procedure or cone biopsy), or ablation like cryo- or laser therapy. As with all cancers, early detection and management can prevent the development of invasive cancer.
Good news: we can prevent cervical cancer (and other cancers) through vaccination!
Have you heard the adage: an ounce of prevention is worth a pound of cure?
In the case of HPV-associated cancers, that is absolutely true. The reality is, we can actually prevent that entire process I described above from ever occurring, through HPV vaccination.
As I mentioned, HPVs are categorized into non-oncogenic and oncogenic. We have several HPV vaccines, and they all protect us against the oncogenic HPV types that are most commonly associated with cancers.
3 vaccines have been licensed by the FDA but Gardasil 9 is most commonly used. Gardasil 9 prevents from type 6, 11, 16, 18, 31, 33, 45, 52, 58, which are the HPV types that cause the most HPV-associated cancers.
HPV types 16 and 18 cause about 70% of cervical cancer as well as oropharyngeal cancers (cancers of the back of the throat, including the base of the tongue and tonsils), anal cancer, penile cancer, vaginal cancer and vulvar cancer. HPV types 31, 33, 45, 52 , 58 account for an additional 10% to 20% of cervical cancers. HPVs type 6 and 11 cause 90% of genital warts.
HPV vaccination works extremely well and is one of the first vaccines that helps protect individuals from getting different types of cancers (in addition to the hepatitis B vaccine, another one that prevents cancers!)
HPV vaccination has the potential to prevent more than 90% of HPV-attributed cancers.
Everyone should get vaccinated for HPV, regardless of gender.
Everyone has at least one body part or organ system that can develop HPV-associated cancer, and more than that, people can transmit HPV to others, which can cause cancer in those individuals.
Gardasil®9 is approved by the FDA for use in males and females ages 9 to 45.
The CDC’s Advisory Committee of Immunization Practices (ACIP) recommends that all girls and boys get vaccinated at age 11 or 12, or as early as age nine, and that adolescents and young adults ages 13-26 be given a “catch-up” vaccination. The FDA expanded its approval of the HPV vaccine to include adults ages 27 to 45. ACIP recommends that adults ages 27 to 45 who have not been properly vaccinated who may be at risk for new HPV infections consult with a medical professional about receiving the vaccine.
HPV vaccine offers long-lasting protection against both HPV infection, HPV disease, and cancers that are caused by HPVs. The greatest benefit from HPV vaccination is getting protected before you are sexually active and potentially exposed to any HPV strains, but there is still a benefit to getting vaccinated later on, if you didn’t receive it as an adolescent. Remember, the vaccine protects against multiple types of HPV, all of which can cause cancer.
HPV vaccination prevents cancer: global data shows this.
A recent study from Scotland, published in January 2024, further supports the benefit of HPV vaccination. Scotland implemented their national HPV vaccine program in 2008. Recommendations included routine vaccination of girls aged 12 or 13 and an initial 2-year catchup for girls aged 14 to 18 years. From cervical cancer screening records among women born from January 1988 to June 1996, they found that there were no cases of invasive cervical cancer among women who were vaccinated against HPV when they were 12 or 13. Among women who were vaccinated between 14-22 years old, there was still a substantial benefit.
This is consistent with another study from 2019 that demonstrated an 89% reduction in invasive cervical cancer or carcinoma in situ
Similarly, a study from Sweden in 2020 agrees with this. HPV vaccination at an earlier age offers the most robust protection against invasive cervical cancer, but vaccination offers a benefit regardless.
Vaccination before any potential HPV exposure offers the best protection
Vaccination is a prevention, not a cure. HPV vaccination stimulates the body to develop memory immunity against HPV, specifically the types covered in the vaccine. Upon a future exposure with HPV, this memory immunity and the neutralizing antibodies produced as a result bind to the virus and prevent it from infecting cells. The current HPV vaccines are based on virus-like particles (VLPs) formed by HPV surface proteins. They are not infectious, as they lack the virus DNA.
Vaccination against HPV is critical, and it is more important to get vaccinated before any possible exposure. Preventing infections also means preventing future precancers and cancers, and that isn’t just cervical cancers, but also anal, penile, vaginal, vulvar, and oropharyngeal. While cervical cancer can be detected early via screening test, other cancers caused by HPV might not be detected until they are more serious.
HPV vaccines are safe and effective. More than 135 million doses have been administered in the USA, and we have robust longitudinal data that demonstrate the full scope of HPV vaccination benefit, with long-term evidence showing the impact it has on cancer prevention as well.
If you know someone who is hesitant or resistant to the HPV vaccine, please send them my way; I’d be happy to address legitimate concerns.
As always, thanks for joining in the fight for science!
Thank you for supporting evidence-based science communication. With outbreaks of preventable diseases, refusal of evidence-based medical interventions, roadblocks to scientific progress that improve food and crop sustainability, it’s needed now more than ever.
Yours in science,
Andrea