Covid Catch-Up: What You Should Know
A summer surge is driven by human behavior, viral evolution, and low vaccination rates.
By popular demand, today’s newsletter is an update on the state of affairs of COVID-19. I have a different piece in the works on long COVID and other post-acute sequelae, so don’t be alarmed that those topics aren’t covered here!
With this, my goal is to provide a quick rundown of key details, things to note, and address confusion that has been born from other SciComm accounts that may have provided some inaccurate information.
We are currently experiencing a surge of COVID-19 cases
All metrics demonstrate that the US - and other places globally - are experiencing uptick in case numbers.
Wastewater surveillance, which detects the presence of viral mRNA in sewage on a community level, has been climbing since May 4, 2024. We aren’t at the levels nationally that were recorded during the winter 2023 holiday season, but we haven’t yet reached the peak.
Wastewater trends correspond to positive tests.
While wastewater surveillance is an early indicator, viral spread is reflected in COVID-19 case rates too. PCR test positivity results reported to health departments demonstrate nearly every US region is reporting increased prevalence of COVID-19.
A note: test positivity is the number of positive PCR test results compared to the total number of PCR tests administered.
In particular, test positivity rates have increased the most over the last 4 weeks in HHS region 9, which includes California, Nevada, and Arizona. There, test positivity rates are now nearing 16%, with a national average currently of 11%.
If you look retrospectively, the test positivity rate increase began with the trends currently emerging in the mid-Atlantic, southeast, and western regions, so it is possible the rest of the country will approach those test positivity rates soon.
What does this tell us? More people who are getting PCR tests done under suspicion of COVID-19 do indeed have COVID-19.
So, higher levels of SAR-CoV-2 are being detected in wastewater, and more people are testing positive when receiving PCR tests. How does this relate to illness?
Positive tests and wastewater trends have a relationship with emergency department visits.
Yes, there is an increased percentage of emergency room visits since May 15, 2024, which lags about a week and a half behind the upswing in wastewater viral prevalence.
Currently, 1.6% of ED visits are attributed to COVID-19, which represents an increase of 15.7% of ED visits compared to previous weeks.
What does this mean? While ED visits due to COVID-19 are still a small proportion of total ED visits, more people are seeking emergent care due to symptoms or suspicion of COVID.
Confounders include:
Access to other non-emergent medical care. For example, in areas where you might not be able to get to your primary care physician or an urgent care center or walk-in clinic, people may resort to the emergency department as their option.
Media attention can drive behaviors. With news headlines discussing the emergence of new SARS-CoV-2 variants, this can increase the likelihood that someone may seek medical care if they might not have previously.
There is a slight increase in hospitalization rates due to COVID-19.
Increased frequency of ED visits can precede increase hospitalization rates, particularly if we are seeing more severe illness.
There is a slight increase in hospitalization rates over the last 2 months, but as of yet, increase spread is not translating to increased illness.
Current estimates of hospitalization rates are roughly 2 hospitalizations per 100,000, compared to 1.1-1.2 hospitalizations per 100,000 in May.
So if there are 250,000 people hospitalized on any given week, that means 5 of them now would be due to COVID-19, compared to 3 of them due to COVID-19 in May.
I hope this provides some reassurance. Yes, we want to be aware of the surge in cases and viral spread, but it is not leading to substantial upticks in hospitalizations.
Mortality rate due to COVID-19 is relatively stable.
The mortality rate due to COVID-19 has been relatively flat since the winter surge, and overall, has been declining. However, there are still between 100 and 300 deaths per week due to COVID-19, so this is not something to merely brush off.
COVID-19 spread is driven in part by human behavior.
Absolutely, people have COVID-19 fatigue. It’s why I was a bit hesitant to write a newsletter focused on COVID-19; I know that there have been headlines every day for 4 1/2 years on the topic. COVID-19 fatigue is also why complacency related to precautionary measures has increased over time.
That being said, it is unlikely we will see the end of COVID-19 in the near future. We are seeing some patterns in infection and illness emerge: we generally expect surges to appear when people are likely to be spending time indoors and congregating with each other. That includes the winter holiday season and the summer months.
The summer trend is interesting because we see more distinct seasonality with influenza viruses and other respiratory viruses. COVID-19 spread in the summer is driven by people seeking cooler, air-conditioned indoor activities when the heat and humidity gets to be too much. This has occurred in previous years as well.
Will these be the expected patterns as we continue on? It is possible, but these patterns take several seasons to stabilize, so it is a bit too soon to tell.
Do you need to panic about COVID-19? No, but we aren’t using the tools we have available.
First and foremost, vaccination rates are still abysmal, for nearly all demographics. Unfortunately, COVID-19 and the associated vaccines have been incredibly politicized, even more so than the other anti-vaccine disinformation I’ve discussed previously.
Many of the same players are at the center of it: RFK Jr. and Andrew Wakefield continue to elevate and propagate anti-vaccine rhetoric. However, in the case of COVID-19 and mRNA vaccines, there is a larger political structure at play.
I’ll save some of this for another day, but suffice to say that the claims as they relate to COVID-19 vaccines are unfounded. The vaccines have demonstrated significant efficacy, particularly at reducing symptomatic illness, severe illness (including hospitalization), and death.
Unfortunately, only 14.4% of children are up-to-date on COVID-19 vaccines. Only 13.3% of those who are pregnant and 22.5% of adults, collectively, are up-to-date. While the highest risk demographic, adults 75 years and older, have the highest coverage, only 41.5% of adults 75+ are up-to-date.
What does being up-to-date on vaccinations mean?
If you didn’t receive a COVID-19 vaccine after September 2023, you are NOT considered up-to-date.
In September, Pfizer-BioNTech and Moderna released the 2023-2024 formulation, which covers a single strain of SARS-CoV-2, the XBB.1.5 variant. Over the last 4 years of viral evolution through mutation, this vaccine more closely matches the circulating variants.
As such, getting up to date means you will generate broader memory immune protection - both memory T cells and antibodies that can help neutralize virus (see here and here for details about memory immunity and vaccination-associated immunity).
If you are over 65, you are eligible for an additional dose of the vaccine. Because older adults are at higher risk for complications and you experience less robust immune protection as you age (this is called immunosenescence), augmenting that response can help reduce poor outcomes. For those with conditions that lead to different types of immunodeficiencies, you are also eligible for additional doses to offer additional protection.
There will be an updated vaccine formulation for the 2024-2025 season that will be rolled out in the fall. If you are in a high risk demographic or are not up-to-date, you should consider getting a vaccine now, to ensure you have a sufficient interval between now and the fall vaccine schedule, and the predicted winter surge due to human behavior.
SARS-CoV-2 FLiRT variants KP.3 and KP.2 are predominant.
As viruses are wont to do, SARS-CoV-2 mutates. Mutations are a result of random errors that occur when an organism replicates. In the case of viruses, the speed at which these errors occur is a function of how many hosts they have to replicate in.
This means the more people SARS-CoV-2 infects, the more chances for mutations to occur.
Mutations are completely random, but ones that are advantageous for the virus are likely to stick in the population (yes, this is microbial evolution!)
These advantageous mutations allow viruses to:
Better attach to and infect host cells
Replicate faster and increase the number of viral offspring that can be spread to the next host
Infect a new class of host (for example, a species jump)
Evade host immune defenses
The FLiRT variants have some key mutations in the spike protein that seemingly allow them to evade neutralizing antibodies: the first checkpoint in memory immunity that can outright prevent a virus from latching onto our cells and infecting them (discussed here). This is a similar pattern that was observed with other new variants that drove previous case surges.
The good news? Illness does not appear to be more severe with FLiRT variants.
There are a few reasons behind that, but the biggest one we have control over is memory immunity. While the entire range of neutralizing antibodies we have produced after vaccination (or even previous infections) may not fully inactivate these viruses if we are exposed, memory immunity consists of much more than that. Memory B cells and memory T cells are able to respond more quickly and augment our defenses to eliminate the infection before illness progresses to become more severe.
This is the same phenomenon with influenza viruses and flu vaccines, (discussed here): even if the strain you are infected with isn’t a perfect match to the vaccine strain, your immune system creates a diverse memory, which still offers substantial protection.
This underscores the importance of vaccination, so if you are not up-to-date, you should consider doing so.
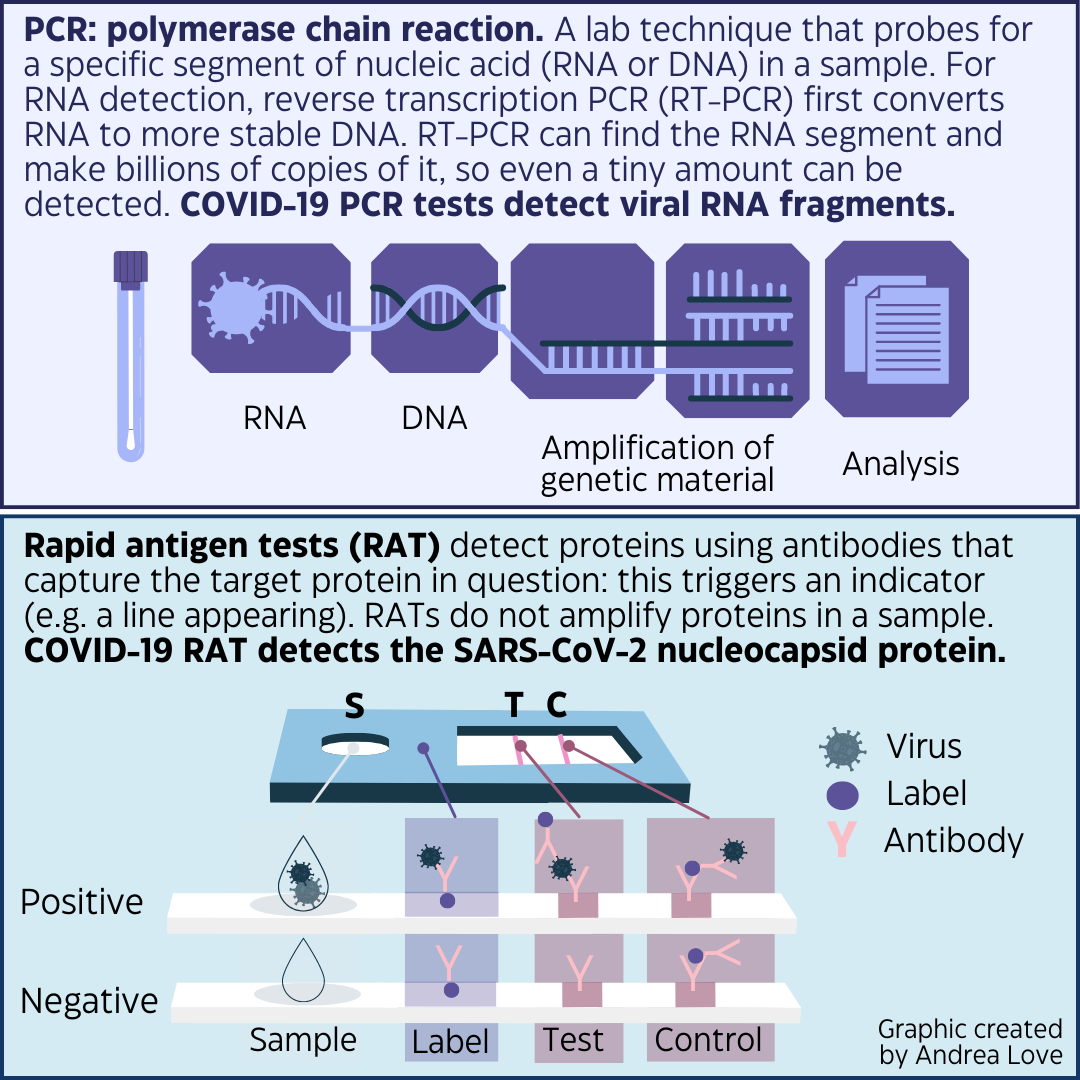
Let’s talk tests. There is still confusion about PCR tests and rapid antigen tests (RAT) for COVID-19.
PCR, officially polymerase chain reaction, is a method to probe for a specific segment of nucleic acid (DNA or RNA) and detect even the smallest quantities using an amplification method. PCR tests for SARS-CoV-2 are very sensitive, but they can also detect fragments of RNA that may be leftover after illness, and not indicate that a person is contagious or has replicating virus in their body.
Rapid antigen tests (RAT) detect a specific protein using an antibody capture technology. They don’t amplify the quantity of protein in a sample, so they are useful to screen for samples that contain the highest levels of protein. In the case of SARS-CoV-2, this would indicate a sample from someone with actively replicating virus, meaning they are contagious.
Rapid antigen tests are a useful screening tool.
Because RATs are not amplifying viral nucleocapsid protein, if the tests detects the presence of it, it is a good indicator that you are contagious in the moment you took the test. As such, if you are actively sick and take a rapid test (these are the ones you can administer at home in about 15 minutes), this should be a signal that you should assume you are contagious and implement isolation protocols.
However, there are some caveats. A negative rapid test result does not mean you aren’t contagious, especially if you have symptoms consistent with COVID-19. Because the detection limit is higher, meaning you need more viral protein in a sample (compared to the level of RNA that can be detected in a PCR test), if you test too early in infection, the viral load may be below the detection level.
What are some next steps if you have symptoms consistent with COVID-19 but test negative with a rapid test?
Consider getting a PCR test done if you want certainty.
Assume you have COVID-19 and isolate accordingly.
Assume you might have COVID-19 OR a different communicable illness (like RSV, metapneumovirus, adenovirus, etc) and still implement isolation precautions.
What should I do isolation-wise if I have COVID-19?
If you recall, CDC updated isolation guidance for respiratory illnesses, which includes COVID-19. These updates are to reflect the window that someone is most contagious with communicable respiratory diseases, and also try to be realistic about the fact that many people cannot or will not be able to isolate for 10-14 days.
Step 1: Stay home when sick until your symptoms improve AND you are fever-free without medication for at least 24 hours.
Step 2: Take additional risk mitigation precautions for another 5 days including wearing a high quality KN95/N95 mask, using rapid testing before interacting with highest risk individuals.
In a perfect world? I would recommend using rapid testing to test OUT of isolation.
Rapid tests are going to detect samples that are from those who are most contagious. If you tested positive with a rapid test during your illness, a negative test following that, which can be from 4-15 days in the course of illness, is a useful indicator that you’re no longer carrying enough virus to successfully infect someone else. Ideally, 2 negative tests in a row are best, as there are places where self-administered tests can be prone to errors.
Unfortunately, the government no longer funds the free at-home tests, so if you are unable to afford them, your insurance or employer does not reimburse or expense them (if you don’t know if your employer will cover these, it is worth asking!), then you may not have access to sufficient supplies of rapid tests.
In that case, you should, at a minimum, wear an N95 for at least 5 days after you’re symptom free when you’re indoors and around other people.
Paxlovid appears to only be beneficial for select individuals.
If you do get COVID-19, nothing substantial has changed about symptom and treatment guidance. Paxlovid is still available by prescription and is most helpful for individuals at high risk (particularly adults over 65), and those who are not current on vaccinations. Older adults have reduced memory immune protection due to immune system aging and the fact responses get less potent. Individuals who are not up-to-date on vaccines have reduced memory immunity as they did not have recent priming of that memory response via vaccination.
If you are fully vaccinated, recent data suggest that Paxlovid does not shorten symptom duration or reduce long COVID symptoms.
The best thing to do to protect yourself? Stay up-to-date on vaccinations.
COVID-19 is not going to disappear anytime soon.
With this summer surge, you don’t need to panic, but you do need to be practical and cautious. The more people get complacent and don’t implement basic risk mitigation measures, the more SARS-CoV-2 is likely to mutate and continue to drive surges and spread among our population.
This is the nature of the host-pathogen arms race: who will evolve first? In the case of humans versus viruses, it is almost always the virus. That’s why we must use our knowledge, our tools, and our technologies to try to outwit them.
Thanks for joining in the fight for science!
Thank you for supporting evidence-based science communication. With outbreaks of preventable diseases, refusal of evidence-based medical interventions, propagation of pseudoscience by prominent public “personalities”, it’s needed now more than ever.
Stay skeptical,
Andrea
“ImmunoLogic” is written by Dr. Andrea Love, PhD - immunologist and microbiologist. She works full-time in life sciences biotech and has had a lifelong passion for closing the science literacy gap and combating pseudoscience and health misinformation as far back as her childhood. This newsletter and her science communication on her social media pages are born from that passion. Follow on Instagram, Threads, Twitter, and Facebook, or support the newsletter by subscribing below:








Thank you for this post, especially for the concise explanation of and practical advice regarding the two types of tests --- very useful for future reference when one needs to test but cannot quite remember these essential facts.