Chronic Lyme Disease: fake diagnosis, but it's more complicated
"Chronic Lyme disease" is a medically discouraged term, but is used by media outlets and activist organizations to explain an array of generic symptoms.
“Although Lyme disease is a public health concern, extensive publicity has resulted in a degree of anxiety about Lyme disease that is out of proportion to the actual morbidity that it causes.”
If you don’t follow me on Instagram or Facebook, you might have missed that last week, I was in DC at the Department of Health and Human Services for the Public Roundtable for the National Strategy on Vectorborne Diseases. This is a multi-pronged project created by an interdisciplinary team to address tick- and mosquito-borne diseases in the US.
While many people focus on Lyme disease, few realize there are vector borne diseases of significantly greater concern for ecology and public health. Lyme is the most common VBD in the US, but it does not cause the most severe illness. Unfortunately, because of public attention and activism born from pseudoscience, it is plagued with misinformation and undue fear. (I wrote about some of the converging factors in one of my Skeptical Inquirer columns).
The National Strategy on Vector-borne Disease is bold
The National Strategy on VBDs aims to address multiple areas: improved prevention, detection, education, surveillance, testing, and treatment. This includes mosquito-transmitted infections like Dengue, currently causing outbreaks in Puerto Rico and West Nile virus, which has pockets of outbreaks periodically, tick-transmitted infections like Rocky Mountain Spotted Fever, which has a mortality rate of up to 40% if untreated and is disproportionately impacting native populations in the southwest, and Lyme disease, which is almost never fatal (a handful of fatalities have been linked to rare cardiac-related complications over the last several decades), but is the most common VBD in the US.
Pathogens transmitted by vectors often have complex survival and replication strategies, because they have to live inside different environments. For example, a midgut of a tick has a very different temperature and nutrient gradient than the tissue or blood of a mammal. In addition, there are multiple layers of participants that are involved when talking about a vector-borne disease: collectively called the enzootic cycle.
When addressing tickborne diseases, all of these factors play a role:
Controlling the vectors themselves and preventing vector bites
Controlling reservoir hosts
Addressing the ecology the vectors and the pathogens live in and their interactions with humans
Understanding pathogen survival and transmission dynamics
Understanding infection and disease process in a human
Characterizing symptoms and etiology of illness
Diagnosing illness correctly
Treating infection and/or managing symptoms
Educating the public and healthcare providers on correct information
Improving surveillance of vectors, pathogens, and incidence of illness
and more…
In addition to the overall priorities and goals, there are (4) main targeted public health outcomes (and no, they don’t ONLY relate to Lyme disease). They include:
Eliminate deaths from Rocky Mountain spotted fever in Arizona tribal communities by 2025.
Eliminate sustained local spread of dengue by 2035. Sustained is defined as having more than 10 related cases in one jurisdiction.
Reduce the number of Lyme disease cases (laboratory confirmed) 25% by 2035, compared to 2022.
Reduce the annual number of West Nile virus neuroinvasive disease cases to below 500 by 2035.
The problem? Misinformation and Lyme pseudoscience derails legitimate science.
Yes, a week prior to this meeting with HHS, CDC, DoD, USGS, and other governmental agencies to review and discuss the priorities with individuals involved in vector-borne disease, TIME published a piece with the title “Long Dismissed, Chronic Lyme Disease Is Finally Getting Its Moment” which propagated many of the same false claims that have pervaded the Lyme field since the 1980s.
In fact, these myths and misconceptions were exactly why the American Lyme Disease Foundation (of which I am the current Executive Director) was created in the 1990s: a consortium of legitimate entomology and infectious disease experts aimed at combating the misinformation spread by activist organizations that mislead the public and impact law and policy.
So I reached out to the TIME author, interestingly the same women who wrote the extremely complimentary piece on Andrew Huberman last year. I provided context and history for Lyme pseudoscience, problematic history with the individuals she quoted in her piece (including the “documentarian” Lindsay Keys), and the fact that this type of media coverage does more harm than good. She acknowledged my message and “appreciated the feedback” - seemingly the same canned reply when I contacted her about the elevation of Huberman - and we’ve seen where that has gotten us.
Chronic Lyme Diseases is a medically discouraged term and media outlets saying it is getting “its moment” are causing harm to public health.
Chronic Lyme disease is one of the more controversial topics in infectious diseases, in that there is a faction of people who have very passionate feelings about the topic of Chronic Lyme Disease, to the point that it becomes part of their identity. The most interesting part (to me) about this is that there are so many other infections/illnesses with a much larger morbidity and mortality burden. Lyme disease is not a fatal illness and has very effective treatments.
“Chronic Lyme disease” is a nonspecific diagnosis without a consistent definition that has been given to patients with various generic symptoms that *could* be associated with infection with B. burgdorferi. Many people diagnosed (either by a “Lyme literate” physician - more on this topic soon, or by themselves), state they have chronic Lyme because they have symptoms such as fatigue and pain.
In fact, credible expert organizations including the Infectious Disease Society of America and the CDC DISCOURAGE the use of the term, because it is used to suggest that there is an ongoing infection with a bacterial pathogen.
To be clear: there is no human evidence that Lyme disease establishes a persistent or chronic infection.
But let’s take a step back for a minute. Remember, Lyme disease is caused by the bite of an infected black-legged tick, which, if feeding on a human for >24 hours, can lead to the bacteria Borrelia burgdorferi to be deposited into the skin. The vast majority of infections are halted right there in the skin. In small proportions of cases (~20% or less), certain strains of the bacteria can escape the skin near the tick bite and spread to areas such as the joints, central nervous system, and the heart to cause symptoms of disseminated Lyme disease.
Importantly, this is a bacterial infection. These bacterial infections are treated effectively with specific courses of antibiotics.
For localized Lyme disease, the treatment is Doxycycline for 10 days, Amoxicillin for 14 days, or Cefuroxime for 14 days. For disseminated Lyme disease that presents as arthritis, treatment is 28 days of any of those three, or 14-28 days of IV Ceftriaxone. For disseminated Lyme disease that presents with neurological symptoms (such as facial weakness/palsy), treatment is Doxycycline for 14-21 days or IV Ceftriaxone for 14-21 days. And for the very rare instances of disseminated Lyme disease that presents with cardiac symptoms, treatment is 14-21 days of Doxycycline, Amoxicillin, or Cefuroxime for mild symptoms, and 14-21 days of IV Ceftriaxone for moderate-severe cases.
There is no benefit to taking extended courses of antibiotics if someone has been led to believe they have a chronic infection, and in some instances, it can actually cause serious harm (more on this in a moment). Numerous clinical trials have investigated this and determined there is not even an improvement in quality of life with extended courses of antibiotics.
Borrelia burgdorferi do not form biofilms, ‘persister cells’, or become dormant or latent in the body and hide out from antibiotics or our immune system. Studies that claim otherwise have no conclusive evidence to present. As such, courses of these antibiotics kill all the bacteria and eliminate the infection.
There is no evidence of chronic Lyme infection in humans.
In fact, even without antibiotic treatment, most infections would self-resolve (i.e. be cleared by our immune system) anyway. This term, because it is applied to a wide array of nonspecific symptoms has unfortunately provided a rallying point for people with similarly vague symptoms seeking a concrete diagnosis, whether they had Lyme disease or not. Studies trying to make claims to the contrary are not assessing human evidence, and frequently are not assessing viable bacteria even in animal models of Lyme.
Here’s where it gets tricky (and why the notion of chronic infection has been successful):
About 10% of people who had a legitimate B. burgdorferi infection report fatigue, musculoskeletal pain, and insomnia that may continue for more than 6 months after the infection has resolved. This is NOT chronic Lyme disease but rather, post-treatment Lyme disease syndrome (PTLDS).
Post-treatment Lyme disease syndrome means residual symptoms persist after antibiotic treatment has eliminated the infection. It’s a little bit like “long COVID”: officially termed Post-Acute Sequelae of SARS-CoV-2 infection (PASC). Sequelae is the key term here: this means resulting consequences of past injury or disease. Persistent symptoms in these instances are NOT due to bacteria that are still in your body: it is due to potential tissue damage before the infection was cleared and the resulting inflammatory response that can take time to return to baseline following infection in some people.
In addition, because many people self-diagnose or use fraudulent tests to diagnose themselves with Lyme, the number of people believing they have chronic Lyme disease is well over the true number of people that are even infected with B. burgdorferi, including in places where these bacteria and the ticks that transmit them do not even exist.
Across the board, 15% of adults report unexplained fatigue and 30% of adults report unexplained chronic pain.
Unfortunately, as these symptoms could be associated with B. burgdorferi infection (as well as a myriad of other things), these symptoms are often inappropriately attributed to ‘chronic Lyme disease’.
Many patients whose symptoms overlap heavily with those of PTLDS include those with osteoarthritis, rheumatoid arthritis, degenerative diseases of the spine, neurologic diseases, including multiple sclerosis, demyelinating diseases, amyotrophic lateral sclerosis, neuropathies, and dementia, or even depression.
There is no epidemiologic evidence that these diagnoses cluster in regions with high Lyme disease transmission. There is no association between diagnoses such as multiple sclerosis, amyotrophic lateral sclerosis, or rheumatoid arthritis and Lyme disease. These medical conditions do not arise concurrently with symptoms of disseminated Lyme disease (such as Lyme arthritis), and there is no robust and high-quality evidence associating any of these diagnoses with infection by B burgdorferi. Although there can be SYMPTOM overlap between Lyme disease and other conditions, these conditions are distinct from each other.
Patients and patient activist organizations claim that their symptoms are the result of a persistent Lyme disease infection that has gone undiagnosed, even though many of these patients show no objective evidence of a previous infection.
Are these symptoms real? I’m sure they are. But attributing them to chronic Lyme, particularly if the patient has no credible indication they were ever infected, misleads them and can cause them more harm if they don’t get appropriate treatment for what is causing their symptoms.
These medically unexplained symptoms and associated media coverage have led to the rise of adoption of this identity of having “chronic Lyme disease”, and Lyme is used as scapegoat for other ailments because of the non-specific symptoms and many people’s inability to notice the EM lesion (which presents within the first 1-2 weeks of infection and occurs in 60-80% of cases). This means that people may be ignoring other legitimate medical issues that are causing these generic symptoms, as they believe they have a chronic infection with B. burgdorferi instead.
More worrisome is that people who are led to believe that they do have a chronic Lyme infection end up taking unapproved and unproven treatments, which can be dangerous. There are no data that tie these physical symptoms to ongoing infection, and prolonged or repeated courses of antibiotic therapy are emphatically not recommended.
Treatments offered for chronic Lyme disease, such as prolonged antibiotic or immunoglobulin therapy, lack data supporting effectiveness and are not recommended. In fact, long-term IV antibiotics and “holistic” remedies have been associated with dangerous infections.
Unfortunately, the rise of social media and public legitimization of “Lyme specialists” (who are not trained in infectious diseases) has led to huge increases in long-course antibiotic treatments. Comparing 2004-2006 and 2010-2012, there was a 50% increase in long-course antibiotic therapies prescribed for Lyme disease.
Doctors who prescribe these treatments don’t follow recommended treatments and evidence-based guidelines and frequently diagnose Lyme disease even if the FDA-approved blood tests are negative.
There is an entire fringe of clinicians who call themselves “Lyme literate” that propagate these falsehoods, and they personally profit by prescribing these unproven treatments that are not covered by insurance and are extremely costly. These clinicians typically don’t even have formal infectious disease training, and are preying on people who simply want a diagnosis to their ailments. (More on this topic soon).
Alternative treatments promoted for chronic Lyme are not without risk.
Clinicians, health departments, and patients have contacted CDC with reports of serious bacterial infections resulting from treatment of persons who have received a diagnosis of chronic Lyme disease. Many of these cases illustrate complications resulting from unproven treatments, including septic shock, Clostridium difficile colitis, osteodiscitis, abscess, and death.
These “treatments” have no evidence that they improve quality of life. Many of these individuals were misdiagnosed as chronic Lyme when they have other medical issues: depression, MS, etc. It’s important to remember that Chronic Lyme is not a medical diagnosis.
Seeking help from alternative care providers is associated with skepticism about conventional medicine and makes these individuals susceptible to false claims.
These include psychological factors (such as hope, or wishful thinking), distaste for conventional authority figures (such as physicians) or for conventional science, and vigorous marketing by those promoting them. As this study illustrates, practitioners of unorthodox alternative therapies specifically target their marketing to the group of patients who believe they have Lyme disease.
If you see anyone promoting these treatments for Lyme, please beware:
“Oxygen therapies” such as hyperbaric oxygen, hydrogen peroxide, or ozone
“Energy and radiation therapies” such as Ultraviolet light, Photon therapy, magnets, saunas/steam rooms, and “cold” lasers.
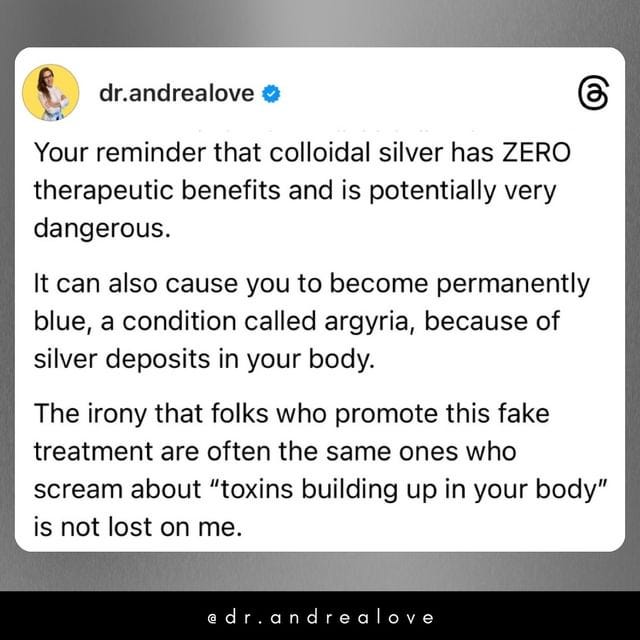
“Metal/chelation therapies” such as mercury chelation and removal, Dimercaptosuccinic acid (DMSA), Alpha lipoic acid (ALA), Removal of dental amalgam, Colloidal silver, and bismuth.
“Nutritional supplements” such as Vitamins C and B12, Herbs, Garlic, cilantro, Chlorella, Sarsaparilla, Andrographis, Turmeric, Olive leaf, Glutathione, and Fish oil
“Biological and pharmacologic agents” such as Urotherapy (urine ingestion), Enemas, Bee venom, Hormonal therapy, Cortisone, Naltrexone, Sodium chlorite (bleach), Intravenous immune globulin (IVIG), Synthetic thyroid hormone, and apheresis.
These are only a selection of things promoted to treat a supposed chronic Lyme infection. Not only are these potentially dangerous, there is NO biological plausibility as to why any of these treatments would be effective to begin with.
There is ongoing research to better characterize the pathology of PTLDS in individuals who present with symptoms beyond acute infection, but these treatments are not the answer. These products—available online or from some health care providers—may be dangerous, deadly, or simply a waste of money. (many aren’t covered by ins. b/c they aren’t medically proven). Legitimate experts routinely express concern that many patients are improperly diagnosed and are receiving treatmenst, i.e., long-term antibiotic therapy, that will do them more harm than good.
Yes, it is frustrating when you have physical symptoms that match those of Lyme with no official label to put on them, but chronic Lyme disease is a label that is used to exploit you when you are vulnerable. It is not the solution. Please, be wary of clinicians, alternative practitioners, and others who promote this.
Thanks for joining in the fight for science!
Thank you for supporting evidence-based science communication. With outbreaks of preventable diseases, refusal of evidence-based medical interventions, propagation of pseudoscience by prominent public “personalities”, it’s needed now more than ever.
Your local immunologist,
Andrea
“ImmunoLogic” is written by Dr. Andrea Love, PhD - immunologist and microbiologist. She works full-time in life sciences biotech and has had a lifelong passion for closing the science literacy gap and combating pseudoscience and health misinformation as far back as her childhood. This newsletter and her science communication on her social media pages are born from that passion. Feel free to follow on Instagram, Threads, Twitter, and Facebook, or support the newsletter by subscribing below: