Autoimmune diets are not based in science
Steer clear of unfounded rigid elimination diets that promise to cure an array of ailments
The Autoimmune Protocol (AIP) diet or broadly, autoimmune diets, are marketed as stricter versions of the paleo diet (an eating plan modeled on supposed prehistoric human diets). Paleo has been made very popular by celebs including Gwyneth Paltrow, Blake Lively, Matthew McConaughey, Jessica Biel, Miley Cyrus, Uma Thurman and Jack Osbourne, and many more. Remember: these individuals are not trained scientists or clinical experts in nutrition or immunology, so please be wary of taking advice from celebrities.
The growing popularity autoimmune diets started around 2010, and uses the principle of elimination diets. Elimination diets are used clinically to identify possible allergies or food intolerances. These are conducted under the supervision of allergists/immunologists, but these follow specific methods in order to determine if a food is a potential allergen or you have a digestive issue related to one.
As with many pseudoscience topics, a grain a truth is used to wildly exaggerate. In this instance, the clinical utility of elimination diets has been co-opted for unsubstantiated diagnoses like ‘food sensitivities’, leaky gut syndrome’, and even weight loss. And now it is being promoted to cure or alleviate symptoms of ‘inflammation’ or autoimmune disorders.
This because there is a poor understanding of what inflammation actually means.
People mistakenly confuse the fact that in certain chronic diseases, a hallmark of pathology is inflammation. That does not mean that inflammation causes the disease. It usually means that there is an immune system component to the disease, and the immune system regulates our inflammatory (and anti-inflammatory) responses.
There is no evidence that rigid diets such as these help to resolve or cure autoimmune disorders.
Autoimmune disorders are incredibly diverse, so why would a singular diet ‘cure’ them?
There are currently about 80 identified AIDs. Many have genetic linkages, some are related to past viral infections, other environmental factors, and epigenetics. Autoimmunity is when our body - usually a component of our immune system - reacts inappropriately to something ‘self’, and that creates tissue damage, cell death, and ultimately, symptoms of disease. Normally our immune system exhibits tolerance toward our own cells, but during autoimmunity, these processes go awry.
A few examples:
Type 1 diabetes is autoimmunity directed at pancreatic islet cells. As a result, our immune system destroys cells responsible for producing insulin.
Systemic lupus erythematosus (SLE/Lupus) is autoimmunity directed at a wide array of tissues in the body, joints, skin, brain, lungs, kidneys, and blood vessels.
Celiac disease is autoimmunity/immune reaction triggered by T cell responses against gluten (protein found in wheat, barley, and rye) in the small intestine.
Hashimoto’s thyroiditis is autoimmunity directed at thyroid cells, which damage cells and reduce production of thyroid hormone, leading to functional hypothyroidism.
Vitiligo is autoimmunity directed at melanocytes (pigment cells) in skin. Results in loss of pigmentation in patches around the body.
These are all VERY different in causes, symptoms, pathology, and disease management. So why would a singular diet ‘cure’ these? The answer: it wouldn’t.
How did the autoimmune diet come to exist?
The autoimmune protocol diet has been attributed to Loren Cordain, PhD, starting in 2002 when he wrote his first book on the topic “The Paleo Diet.” Loren has a PhD in exercise physiology, and has no peer-reviewed publications in the field of nutrition or immunology. However, he claims he “discovered” certain foods trigger inflammation in people with autoimmune disease.
Robb Wolf outlined the restrictive “autoimmune protocol” in his book, The Paleo Solution, introducing it as an elimination diet. Sarah Ballantyne, PhD, also known as the “Paleo Mom”, wrote about it in her book, The Paleo Approach. Sarah Ballantyne is considered by many who are actually trained in nutrition and immunology to be the one who brought this pseudoscience diet into the mainstream. (Another note: Sarah has a PhD in biophysics, not immunology or nutrition).
These books, not robust scientific studies, have made the diet very popular.
Unfortunately these individuals have used the “appeal to false authority” logical fallacy to try and cultivate credibility behind their doctoral degrees.
Their overarching claims suggest that “processed foods” cause causes leaky gut and inflammation.
Inflammation is a frequently misused term in the nutrition field by those who do not understand it.
Inflammation occurs anytime we eat anything.
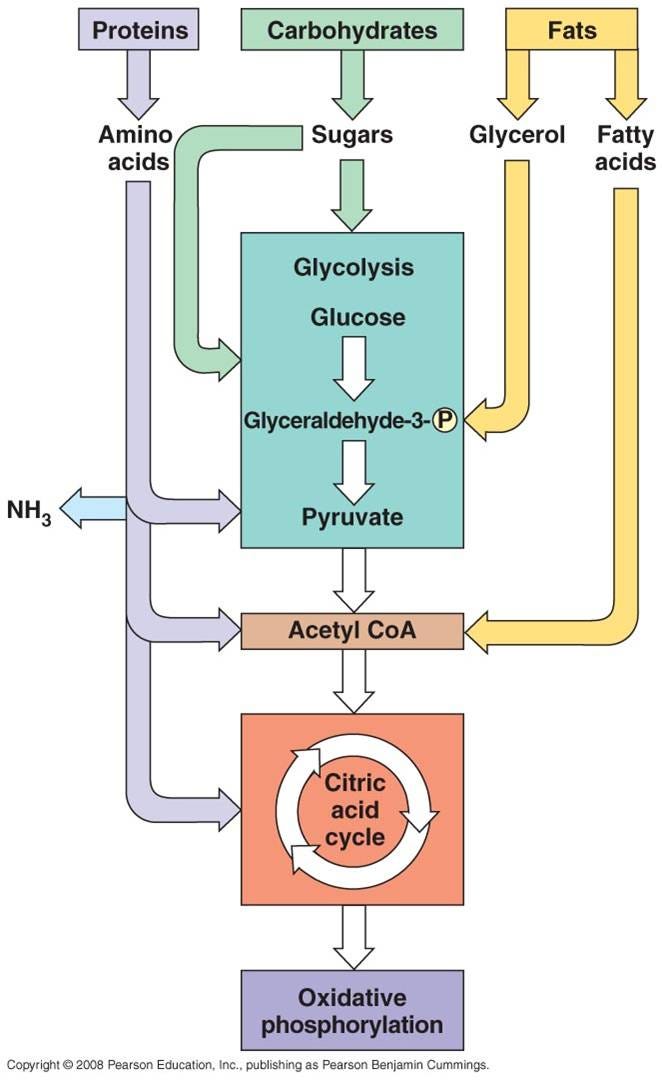
Anytime we eat anything, our body digests those food products into macromolecules, which are further broken down into usable energy components shuttled into our cellular respiration pathway, which is how we convert food into ATP, the usable energy form for our cells.
That is true whether we are digesting carbohydrates, proteins, or fats.
This process is broadly divided into 3 steps: glycolysis→ the citric acid cycle → the electron transport chain and oxidative phosphorylation. Depending which macromolecules involved, their subunits will be shuttled into these pathways at different steps.
During this process of cellular respiration, inflammation occurs.
Literally, everything we eat causes ‘inflammation’ because it is a catabolic process (the process of breaking down things) that creates byproducts and releases energy. Indeed, providing energy sources to our immune cells in order to exert basic functions also creates inflammation.
During cellular respiration, we produce things such as free radicals and reactive oxygen species. These are critical for key physiological processes, but too many can also cause DNA damage and other dysfunction. Of course, these concepts have also been misunderstood and co-opted to make false claims. The important thing to remember is that everything in our bodies is about balance and homeostasis, and these processes are tightly regulated by mechanisms in our bodies, not by a restrictive diet.
(A free radical is an atom, molecule, or ion that has at least one unpaired valence electron, making molecules highly reactive. ROS are highly reactive, oxygen containing molecules that are the result of an incomplete reduction of molecular oxygen in the cell.)
What is inflammation scientifically?
Inflammation, simply put, is our body’s immune response to any stimulus or insult. These can include physical wounds, infection, recovery after exercise, and yes, digestion. Inflammation is essential for life: without these processes, we would be dead. The immune system tightly regulates inflammatory and anti-inflammatory processes: too much of ‘either’ is not ideal.
So why are we trying to avoid ‘inflammation’?
There’s no good reason, and the concept of inflammation as a legitimate scientific process has been co-opted to promote pseudoscience without data. This is a very similar phenomenon to other ‘fad’ pseudoscience topics such as leaky gut syndrome, food sensitivities, and others.
Nutritional patterns collectively termed the “Western diet” include high-fat/cholesterol, high-protein, high-sugar, and excess salt intake, as well as frequent consumption of processed and ‘fast foods’ have been identified to promote obesity, metabolic syndrome, and cardiovascular disease. (A caveat: the terms processed, fast food, and junk food have zero scientific standardization and are frequently used to foment fear. More on that to come!)
We know that is because these are high calorie, low nutrient foods that have always been recommended to consume in moderation, not because of a singular food type that is uniquely promoting ‘inflammation.’
Of course, people have misunderstood and misrepresented this to mean that there is some ‘opposite’ diet that can manage diseases including autoimmune disorders. It is important to remember that immunology and the etiology of autoimmune disorders is incredibly complex, and these metabolic and immunologic mechanisms are being intensively explored.
The autoimmune diet is promoted by unqualified individuals and is not supported by trained professionals.
The premise of diet involves staged elimination of food groups that may be associated with immune stimulation and intolerance, maintenance of the eliminated foods, followed by staged reintroduction of certain foods or food groups over time. The new fad is to recommend this diet for people who suffer from autoimmune disorders (but this is NOT endorsed or recommended by trained professionals).
While this diet is touted to involved phases, since this is not a clinically supported pattern, most people who follow it simply avoid all of the foods claimed to be ‘bad’.
Broadly though, most AIP plans say you can eat:
Vegetables, except those from the nightshade family (tomatoes, peppers, potatoes, eggplants, etc)
Seafood that are high in omega-3 fatty acids
Fermented foods
All meats, limiting chicken due to high omega-6 content
Special emphasis on organ meats
Small amounts of fruit
Vegetable fats and oils, such as olive, coconut, and avocado oils
Emphasis on consuming glycine rich foods including bone broth
In general, the diet demonizes sugars, even those which are found in healthy foods like fruits and vegetables.
Most AIP plans tell you to avoid:
Nightshades (tomatoes, potatoes, peppers, and eggplants)
Grains (including whole grains)
Legumes
Dairy
Other vegetable oils (canola, rapeseed, corn, cottonseed, palm kernel, safflower, soybean, or sunflower oils)
Coffee
Eggs
Nuts and seeds
Alcohol
Food additives including added sugars, non-nutritive sweeteners, etc.
There are obvious issues with this diet.
Sugar is sugar, no matter the source. All carbohydrates are inevitably broken down into simply monosaccharides to be shuttled into that cellular respiration pathway. Ultimately, sugar from white sugar (sucrose, a 1:1 ratio of glucose:fructose) and sugar from honey (also a 1:1 ratio of glucose:fructose) (or fruits) get processed very similarly by our bodies. Our body doesn’t differentiate the source of a macromolecule.
Many of the things stated to avoid have documented health benefits. Whole grains, legumes, and others are nutrient-dense, have high fiber, and offer many health benefits. Seed oils are not harmful or inflammatory, not matter what “CarnivoreMD” (who is a psychiatrist) tells you. Unfortunately, this diet gained popularity because the creators of it have claimed it helped them personally, and not because there is robust scientific evidence behind it.
Remember: anecdotes are not evidence!
There is no convincing evidence this type of rigid diet is beneficial for anyone, including those with autoimmune issues.
There are very limited studies evaluating the AIP diet and contributions to mediating autoimmune disorders.
A study evaluating AIP for Hashimoto’s found no statistically significant changes in thyroid function or thyroid antibodies. As such, there is no evidence that this rigid diet improves disease status among these individuals.
There is a study that is cited often as evidence for AIP: it showed some improvements for those specifically with inflammatory bowel disease (IBD), but has some very substantial flaws in study design.
Limitations of the study include:
Small sample size (n of 15)
Lack of a randomized trial design involving a control group
Lack of blinding
Potential for selection bias among those enrolling in the study (all of these people were recruited from Scripps Clinic Medical Group Division of Gastroenterology (La Jolla, CA), meaning they already were seeking treatment for some ailment)
Participants never moved away from the elimination phase of the diet itself
Used supplements to correct nutrient deficiencies, and as such, you cannot conclude whether improvements were due to supplements or the diet itself
Even within this trial, several people who voluntarily enrolled left this short-term study, because this diet is so rigid and so restrictive that it is simply not sustainable.
In reality, there is very little data to suggest these rigid diets are effective for any autoimmune disorders: including management of the disease itself, symptom alleviation, and more. More than that, a single (and flawed) study assessing a specific gastrointestinal condition is not generalizable to the wide array of autoimmune disorders that these diets claim to alleviate.
Other data actually demonstrate low fat and high fiber diet improve symptoms of GI issues such as ulcerative colitis (these would be considered versions of the Mediterranean diet, which focuses on plant-forward, fiber-dense, well-rounded plates). This is in direct contrast to many of the claims promoted by the AIP diet.
What about “anti-inflammatory diets” more generally?
These often tell you to include things like fruits and vegetables, seed oils, nuts, lean proteins, fish, etc. Does this sound familiar? This is the definition of the Mediterranean diet (the term used in the scientific literature). Literally, just a well-balanced diet with fiber and containing predominantly nutrient-dense foods.
They tell you to avoid ‘inflammatory foods’ like refined carbohydrates, such as white bread and pastries, fried foods, soda and other sugar-sweetened beverages, red meat (burgers, steaks) and processed meat (hot dogs, sausage), margarine, shortening, and lard. These foods are uniquely inflammatory, but they are calorie-dense but not nutrient-dense foods, and are typically low in fiber and other micronutrients our body utilizes for essential physiological processes.
Feeling better when avoiding these foods has really nothing to do with “inflammation” and more to do with balanced nutrition and a more healthful lifestyle.
The placebo effect is strong among people to undertake elimination diets.
Many people claim they felt better on some sort of elimination diet. First, these claims are typically subjected and about individual perception, but it underscores a key detail about the placebo effect: if you believe you are going to have an unfavorable symptom after eating gluten-containing wheat and you eat a sandwich with that fear in the back of your mind, you may very well experience GI upset.
The problem is that you cannot determine if that symptom is due to a medical issue or due to your fear of that food. Anxiety about a food can produce the exact same symptoms as a digestive intolerance and it's very easy to misdiagnose yourself with an intolerance when the real issue is your fear of certain foods.
But interestingly, when people who believed they had “non-Celiac gluten sensivitity” underwent blinded dietary challenges, they don’t actually report symptoms associated with gluten.
Another thing to consider is that when people implement these types of strict diets, they are also making a conscious effort to improve other things in their life: alcohol intake, exercise, etc. These would be considered confounding variables - in that you cannot parse out which of these factors were really the cause of the perceived improvement being reported.
This is why randomized controlled trials are essentially to account for placebo and other variables and biases that can skew data.
Strict elimination diets are not without risk.
There are some very real risks associated with strict elimination diets, specifically among those with pre-existing medical issues such as autoimmune disorders. Obviously, there are risks of nutrient and caloric deficiencies, especially when omitting entire food groups.
Disease management of one autoimmune disorder like type 1 diabetes is not nearly the same as another like celiac disease.
Type 1 diabetes is managed by glucose monitoring and insulin supplementation, because your pancreatic islet cells do not produce insulin.
Celiac disease is managed by avoiding gluten and gluten-containing foods.
These types of elimination diets also risk the development of disordered eating habits, particularly among those that are predisposed. There are also serious psychological impacts and disruptions in personal life/social life: these diets are so restrictive, many individuals cannot go out to restaurants, eat common meals with friends and loved ones, and more.
Bottom line: There is no body of evidence to suggest that a highly restrictive diet, AIP or otherwise, can help alleviate symptoms of autoimmune disorders, or ‘reduce inflammation’ more broadly.
Please be wary of anyone making these types of broad and generalized claims, and if you are considering something like this, consult trained experts in both nutrition and immunology.
Thanks for joining in the fight for science!
Thank you for supporting evidence-based science communication. With outbreaks of preventable diseases, refusal of evidence-based medical interventions, propagation of pseudoscience by prominent public “personalities”, it’s needed now more than ever.
Your local immunologist,
Andrea